It always seems to start the same way—just a little extra hair on the pillow, maybe more in the shower drain than usual. At first, you brush it off (literally and figuratively). But when your ponytail feels thinner or your scalp peeks through under certain lighting, panic creeps in. For many people (especially women), this sudden shift triggers a spiral of questions: Is it my shampoo? Stress? Or… could it be my medication?
Medication‑induced hair loss, medically called drug‑induced alopecia, is far more common than most patients realize. It can appear subtly, months after starting a prescription, or strike rapidly depending on the type of medication and how it affects your hair growth cycle. Unlike hereditary pattern baldness, which follows a predictable path, this type of hair loss can feel unfair and disorienting.
Here’s the good news: in most cases, it’s temporary. And understanding which medications cause hair loss (and why) can help you work with your doctor to prevent, minimize, or reverse it. In this guide, we’ll break down the top medications linked to shedding, explain the exact biological mechanisms behind it, and share evidence‑backed strategies for recovery.
Why Medications Can Trigger Hair Loss?
Your hair isn’t static—it lives in cycles. At any given moment, about 85–90% of scalp hairs are in the anagen (growth) phase, while the rest are in telogen (resting) or catagen (transition). Medications can disrupt this delicate rhythm in two main ways:
Telogen Effluvium vs. Anagen Effluvium
- Telogen Effluvium (TE) is the most common medication‑related hair loss. It happens when a drug nudges too many hairs into the resting phase, causing diffuse shedding 1–6 months later. Patients notice more strands in the shower or on their pillow, but rarely complete bald spots.
Also Read: What can you do to stop telogen eflluvium?
-
Anagen Effluvium (AE) strikes faster (within days or weeks) because certain drugs, like chemotherapy agents, interrupt hair cell division during the growth phase. Hair can fall out in clumps and may include eyebrows or body hair.
Temporary vs. Permanent Hair Loss
The reassuring truth is that most medication-induced hair loss is reversible. Once the trigger is removed or the body adapts, hair follicles often resume normal cycling. Rare cases of scarring alopecia are linked to specific toxicities or autoimmune responses, but these are outliers supported by limited literature.
The mechanism depends on the class of drug, the dosage, and individual sensitivity. Hormonal medications, blood thinners, and certain antidepressants commonly cause TE, while chemotherapy drugs cause AE.
Do you ever wonder why one friend loses hair on a medication while another doesn’t? Genetics, dosage, and even nutritional status quietly influence that outcome.
10 Common Medications That Cause Hair Loss
Medication-induced hair loss can feel like a cruel twist, especially when you’re diligently following a treatment plan for your health.
Below are the 10 most common medications that cause hair loss and how each affects your hair follicles, the type of shedding they trigger, and whether the effect is usually temporary.
1. Blood Thinners (Anticoagulants)
Blood thinners like heparin and warfarin are lifesaving for people at risk of clots, yet they have a quiet cosmetic tradeoff. These medications often trigger telogen effluvium, where too many hairs shift prematurely into the resting phase. Patients usually notice increased shedding two to four months after starting therapy.
The hair loss is generally diffuse—meaning you’ll see more strands in your brush or shower drain, rather than isolated bald patches. In most cases, the shedding eases once your doctor adjusts the dose or switches you to a different anticoagulant. According to clinical observations published, this side effect is reversible in the majority of patients.
(Important note: never stop blood thinners suddenly; sudden discontinuation can be dangerous.)
2. Antidepressants
Antidepressants—especially SSRIs (like sertraline or fluoxetine), SNRIs, bupropion, and older tricyclics—can quietly thin hair over months. They’re not as dramatic as chemotherapy-induced loss, but telogen effluvium is a documented side effect in some individuals, particularly women.
The shedding usually appears 3–6 months after starting or changing the dose. It may feel subtle at first, but you might notice a widening part or thinner ponytail. While researchers are still debating the precise mechanism, the disruption of neurotransmitter balance appears to affect follicle cycling indirectly.
The good news is… most cases reverse when the dosage is optimized or an alternative antidepressant is chosen. Dermatology case studies and pharmacovigilance data show regrowth typically begins a few months after the trigger is resolved.
3. Birth Control Pills & Hormonal Medications
Hormonal changes are a powerful influencer of hair health, which is why birth control pills, hormone replacement therapy, and even certain fertility medications can trigger temporary shedding. Some pills can tip the balance of estrogen and progesterone in a way that encourages telogen effluvium.
Women who are genetically sensitive to androgens—essentially the hormones that can miniaturize hair follicles—are especially prone. Hair shedding often appears 2–4 months after starting, switching, or stopping a hormonal medication. It may mimic postpartum hair loss, which is also a hormonally driven telogen shift.
Most patients experience regrowth within three to six months after their hormonal environment stabilizes. The key is medical supervision if switching pills or adjusting doses, as abrupt changes can prolong the cycle of shedding.
4. Blood Pressure Medications (Beta-Blockers & ACE Inhibitors)
Drugs like atenolol, metoprolol, propranolol, and ACE inhibitors such as lisinopril help protect the heart but occasionally cause unexpected diffuse thinning. The effect is thought to be linked to telogen effluvium, though the exact biological mechanism remains under investigation.
Hair loss with these medications is uncommon, but when it happens, it usually develops gradually over several months. Patients may notice a reduction in overall hair volume rather than patchy spots. Clinical reviews suggest this type of shedding is reversible once the medication is changed or tapered under a doctor’s supervision.
Anecdotally, some people report that the stress of hypertension itself worsens hair shedding… a reminder that multiple factors often overlap.
Read More: Does blood pressure medication leads to baldness?
5. Acne Medications (Retinoids)
Oral retinoids, particularly isotretinoin (Accutane), are highly effective for severe acne but can have collateral effects on the scalp. Retinoids reduce sebum and influence keratinocyte behavior, which sometimes nudges hair follicles into a telogen effluvium pattern.
Hair shedding on isotretinoin tends to be mild and temporary, though long courses or high doses can make it more noticeable. Research suggests the effect is dose-dependent, and regrowth typically occurs after treatment ends.
Patients are often reassured by dermatologists that post-treatment recovery is the norm. A balanced diet with sufficient protein and careful scalp care can help support follicle recovery in this phase.
6. Cholesterol-Lowering Drugs (Statins)
Statins like atorvastatin and simvastatin have transformed cardiovascular prevention—but in rare instances, they’re linked to hair loss. Reports describe a gradual, diffuse thinning rather than patchy bald spots.
The mechanism isn’t fully understood, though researchers suspect alterations in lipid metabolism or nutrient absorption may disrupt hair cycling. Studies suggest the incidence is low, but for sensitive individuals, it can be distressing.
Most cases improve after a medication switch or dose adjustment. Doctors usually weigh the cardiovascular benefit against cosmetic impact and may recommend supportive strategies like laser phototherapy.
7. Anticonvulsants (Anti-Seizure Medications)
Medications like valproate (Depakote), carbamazepine, and phenytoin have well-documented links to hair shedding. In valproate’s case, studies estimate around 10–11% of users experience hair loss.
These drugs can trigger telogen effluvium by affecting nutrient metabolism—especially zinc and selenium—which are essential for healthy follicle cycling. Shedding usually develops gradually after a few months of therapy.
Once the deficiency is addressed or the medication is changed, regrowth typically resumes. Clinicians often recommend bloodwork to check for deficiencies and may suggest supplementation alongside careful monitoring.
8. Thyroid Medications
Your thyroid hormones play a central role in hair growth. Even medications intended to correct thyroid imbalance (like levothyroxine) can trigger telogen effluvium if the dose is too high or too low.
Hair shedding often becomes apparent 2–3 months after a dosage change, and it can occur in both men and women. This is why endocrinologists emphasize regular TSH monitoring and slow dose adjustments.
Fortunately, once thyroid levels stabilize, the hair cycle typically normalizes. Patients often see regrowth within 3–6 months with appropriate dose management.
9. Chemotherapy Drugs
Perhaps the most recognized cause of medication-related hair loss, chemotherapy induces anagen effluvium, leading to rapid and often dramatic shedding. Drugs like cyclophosphamide, doxorubicin, and taxanes target rapidly dividing cells—which include cancer cells and hair matrix cells alike.
Hair loss can start within days or weeks of treatment. Unlike telogen effluvium, which is diffuse and delayed, anagen effluvium often results in near-total scalp loss and may also affect eyebrows and body hair.
The encouraging part: hair usually regrows after treatment, though texture and color can temporarily change. Supportive options like FDA-cleared laser phototherapy (LPT) may help accelerate recovery, according to emerging clinical research.
10. NSAIDs (Nonsteroidal Anti-Inflammatory Drugs)
Common pain relievers like ibuprofen and naproxen are rarely associated with hair loss, but the link is documented. The mechanism likely involves a mild telogen shift combined with individual sensitivity.
Hair shedding here is usually subtle and temporary. Stopping the NSAID—if medically safe—generally resolves the issue. Because many people take NSAIDs intermittently, the effect may go unnoticed unless use is prolonged.
Safe Steps Before Making Any Changes
Here’s the non-negotiable rule: do not stop prescription medications on your own. Some drugs—like blood thinners or antidepressants—can be dangerous to discontinue suddenly. Instead:
-
Document your shedding pattern (even photos help).
-
Schedule a review with the prescribing doctor.
-
Ask about alternatives or dose adjustments that carry a lower hair-loss risk.
This collaborative approach avoids compromising your overall health while addressing the emotional burden of shedding.
Recognizing and Managing Drug-Induced Hair Loss
Catching medication-related hair loss early can make a real difference. The challenge is… it rarely announces itself with fanfare. Instead, it creeps in—a few extra strands on the pillow, maybe a subtle widening of the part line. Some people only notice after comparing old photos or when a hairdresser quietly points it out.
How to Spot Medication-Related Hair Loss Early?
The first clue is usually diffuse shedding rather than isolated bald spots. You might find extra hair in your shower drain or comb, but the pattern is evenly spread across the scalp. This is a hallmark of telogen effluvium, which tends to appear 1–6 months after starting or changing a medication. In contrast, anagen effluvium, like that seen with chemotherapy, often strikes within weeks and can include eyebrow or body hair loss.
Other subtle signals include:
- A thinner ponytail or visible scalp in bright lighting
- Sudden seasonal-like shedding outside your normal cycle
- No clear link to stress, illness, or diet
Recognizing these patterns allows you to discuss solutions with your physician before panic sets in.
When to Seek Professional Help
If shedding persists for more than a few weeks or feels sudden and severe, it’s time to call a dermatologist or trichologist. They can:
- Examine the scalp for miniaturization or inflammation
- Order lab tests (thyroid levels, ferritin, vitamin D, zinc)
- Differentiate medication-induced loss from other causes, like autoimmune or hormonal conditions
A professional evaluation is also reassuring—you’re not left wondering if it’s “all in your head.”
Treatment and Recovery Options
Once the cause is identified, the next question is always the same: Will my hair grow back? In most cases—thankfully—the answer is yes. Recovery is a mix of patience, targeted support, and sometimes medical intervention.
FDA-Cleared Laser Phototherapy (LPT)
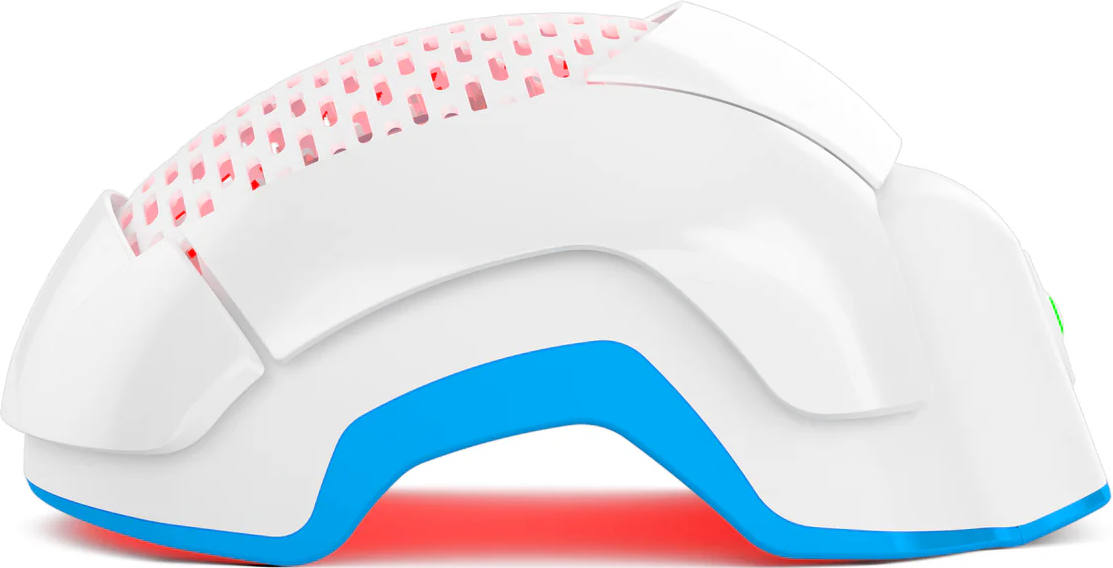
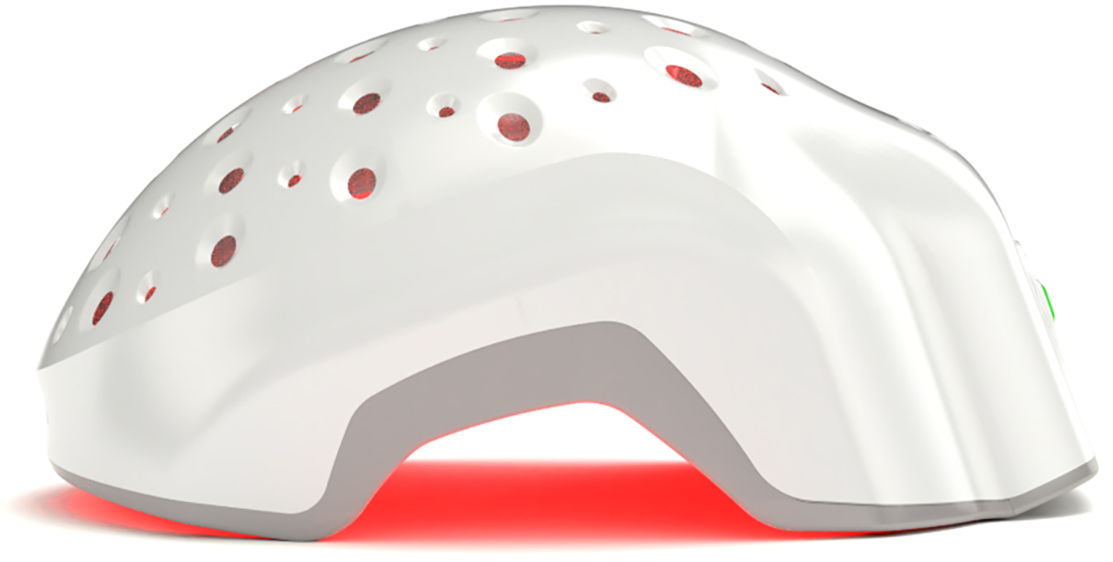
Cold laser phototherapy (LPT) stimulates follicles safely without heat. Class 3R cold lasers, used in medical-grade devices like Theradome, can help restore normal cycling in telogen effluvium cases. Clinical studies, including trials, show improvements in density and regrowth timelines when LPT is used consistently. It’s like “sunbathing for your scalp”… light energy penetrates the tissue to boost cellular repair and blood flow.
Evidence-Based At-Home and Clinical Supports
-
Topical Minoxidil: Often recommended for temporary stimulation, though always under medical guidance.
-
Nutritional optimization: Ensure adequate protein, iron, zinc, and vitamin D. (We avoid the biotin hype—it only matters if you’re truly deficient.)
-
Stress management: Chronic stress can amplify shedding, so scalp-friendly routines like gentle massage and mindfulness help.
Typical Recovery Timeline
Hair cycles move slowly. Even after removing the trigger, regrowth can take 3–6 months before visible density returns. Short, wispy regrowth along the hairline is a promising sign. Patience is part of the therapy—hair grows at roughly 1 cm per month.
Conclusion
Medication-induced hair loss doesn’t just affect appearance—it affects confidence, mood, and identity. Many women, in particular, report that unexpected shedding sparks anxiety or social withdrawal. It’s not vanity; it’s human.
The emotional toll can be eased by knowing three things:
- Most cases are temporary and reversible.
- Abruptly stopping medications is unsafe—always work with your doctor.
- Effective support exists, from LPT devices to dermatologist-guided care.
If you suspect your medication is causing hair loss, start with documentation, consultation, and collaboration. Hair health is part of overall health; prioritizing one without jeopardizing the other is the real goal.
A final note—give yourself grace during recovery. Shedding is unsettling, but with medical supervision, smart scalp care, and time, your hair often rebounds. And if you need a boost while you wait, laser phototherapy and evidence-based interventions can help you feel proactive rather than helpless.
Hair tells a story. This chapter (while frustrating) is almost always temporary.