Yes—kidney diseases can be a factor in hair thinning or shedding. But it’s rarely a direct hit. Often, multiple ripples (nutrient imbalances, anemia, medications, scalp irritation) combine to disturb the hair growth cycle. (We’ll dig into each in a moment.) This isn’t about blaming kidney dysfunction for hair woes; it’s about understanding why your scalp might feel more delicate when kidneys aren’t operating optimally.
(It’s worth repeating—hair loss from kidney ailments isn’t a guaranteed symptom. Yet, if you’re noticing diffuse thinning or brittle strands and you're living with kidney issues, you’re not alone.)
In this post, we explore how kidney dysfunction can influence hair health, backed by research so you see both the biology and practical context.
Understanding the Link between Kidney Disease and Hair Health
At first glance, the kidneys and scalp seem unrelated. But kidneys regulate more than urine… they shepherd nutrient balance, hormone status, and filter metabolic waste. When kidney function declines, systemic stressors begin to accumulate.
Kidney disease can disrupt the delicate orchestration of the hair growth phases—particularly triggering telogen effluvium, a common diffuse shedding pattern.
Healthy hair depends on consistent protein, minerals, and adequate blood oxygen. And this is shaped in part by the kidney‑regulated erythropoietin production. Drift too far off balance, and follicles cycle prematurely into the resting phase, shedding hair in a few weeks.
Add hormonal drift—kidney disease upends cortisol & thyroid rhythms (especially in chronic cases)—and that in turn affects nutrient absorption and scalp circulation. While the cortisol‑hair link is emerging rather than definitive, endocrinology sources hint at real stress‑axis involvement in CKD symptomatic patterns .
In short, hair follicles don’t work in isolation. Kidney ailments quietly influence them through nutrition, anemia, waste buildup, and hormonal dysregulation… leading to thinning, fragility, or diffuse shedding.
How Common Is Hair Loss in Kidney Disease?
Kidney‑related hair loss depends on disease stage and individual vulnerabilities.
Studies report that around 10% of people in end‑stage kidney disease (ESKD) experience notably severe hair loss . That refers to noticeable thinning, not just a few stray hairs. Yet broader chronic kidney disease (CKD) surveys show up to 68% of patients have some form of hair or scalp change (dryness, brittleness, dullness, shedding patterns) most frequently in later stages.
These disparities reflect how researchers define “hair change” and the severity of nephropathy. Early-stage CKD hardly guarantees any hair issues, and many people on dialysis do still retain significant hair density—though texture and sheen often shift.
In one case narrative, a COVID‑infected CKD patient saw diffuse hair loss (even eyebrow shedding). But with dialysis stabilization and correction of anemia, hair began to regrow within months . Such anecdotes don’t represent everyone—but they illustrate that hair health often trails behind kidney health recovery.
So, yes—kidney failure hair loss is real, but it’s not universal. More severe kidney dysfunction correlates with higher prevalence. Yet with proper medical support, many see hair improvement.
Why Kidney Disease Can Cause Hair Loss (Key Mechanisms)?
Understanding exactly why kidney dysfunction might (intentionally or otherwise) leave your hair looking thinner or more brittle involves discussing several biological dominoes. Let’s walk through them.
Nutritional Deficiencies and Protein Malnutrition
Kidney patients (especially those navigating diet restrictions) often end up with suboptimal protein, iron, zinc, selenium, and vitamin D levels. These nutrients are essential for robust hair follicles. When they dip too low (or, in CKD, are filtered poorly and accumulate), follicles lose the ability to cycle through growth phases properly, contributing to telogen effluvium or diffuse thinning. Observational reviews consistently cite nutritional insufficiencies as the primary culprit in CKD-linked hair changes.
Patients may report dull, dry hair—or even see overall loss—not from intentional dieting, but from metabolic imbalances. It’s subtle but tangible.
Anemia and Reduced Erythropoietin (EPO)
Kidneys produce erythropoietin, a hormone critical for red blood cell production, so declining kidney function often leads to anemia. Lower red cell count = less oxygen transported to follicles. That oxygen shortage nudges hairs prematurely into the resting phase, meaning more enters the shed cycle. Studies note that CKD-linked anemia is a frequent trigger for telogen effluvium.
When treated (e.g. with EPO therapy or iron correction), many patients observe a gradual return of hair density after a few months.
Hormonal and Metabolic Imbalance
CKD disrupts endocrine equilibrium… particularly cortisol rhythms and, occasionally, thyroid hormone processing. The result is a stressed internal milieu that can subtly impair hair growth cycles. Though the cortisol‑hair connection in CKD remains partially hypothetical, endocrinology literature suggests a plausible stress-axis involvement.
This hormonal drift may not be dramatic, but over time, cumulative dysfunction weakens follicles’ resilience.
Medication-Related Shedding
Sometimes, the cause is pharmacological. Certain medications commonly used in kidney disease—beta‑blockers, anticoagulants (e.g. heparin), immunosuppressants post‑transplant—are known to accelerate hair shedding or alter growth patterns. Often, the choice to adjust or substitute medication can mitigate further damage.
In many reports, patients notice an initial loss that stabilizes once the drug load changes.
Uremic Pruritus and Scalp Damage
Chronic itching (aka uremic pruritus) is common in CKD. Scratching inflamed skin, over time, can cause physical hair loss from breakage rather than follicular drop. Derm review articles highlight scalp scratching as a local contributor to diffuse thinning.
This can feel frustrating. Your body is shedding, but separately, you might also be wearing away hair shafts via scratching. Two hits.
Autoimmune or Comorbid Conditions
In rare situations, certain kidney diseases have autoimmune roots (for example, lupus nephritis or vasculitis) that may co-occur with alopecia areata—patchy, immune-mediated hair loss. While not typical for most CKD patients, it’s worth noting that overlapping immune triggers can exacerbate hair issues.
What Does Kidney‑Related Hair Loss Look Like?
Folks often describe it as diffuse shedding. Your hair seems to fall more than usual but not in patches. The scalp itself remains intact. Maybe strands feel brittle, dull, or less voluminous. Slow regrowth might follow once systemic issues are addressed.
Hair thinning in this context is generally telogen effluvium, not pattern baldness. That means hair enters a resting phase en masse (like losing 100+ hairs daily, uniformly). Not eyebrows or temples alone. Mostly, the entire scalp.
It’s not dramatic like male‑pattern baldness. It's more subtle, sometimes disheartening when you brush or wash and notice the extra strands. Many kidney disease patients report that hair texture changes—dryness, loss of sheen—even before actual shedding begins.
Importantly, this doesn’t just happen in severe renal failure. Some early‑stage CKD patients still report hair changes (brittleness, dryness). Others only notice visible shedding after dialysis or transplant. (We circle back to this in treatments.)
Can Hair Loss Improve After Treating Kidney Disease?
Yes—sometimes quite markedly. But it’s rarely immediate, and often hinges on how thoroughly underlying factors are corrected.
Treating anemia (via EPO or iron supplements) can restore oxygen flow to follicles. Many patients observe a gradual increase in hair density—sometimes within 3 to 6 months after stabilization .
Similarly, once nutrient levels are brought into balance under medical supervision, hair strength and shine often return—though repletion in CKD is delicate, because excessive supplementation can strain remaining kidney function.
Dialysis can paradoxically help. Fence-sitting? Maybe at first you're still thinning—but stabilization tends to follow as toxin buildup reduces. Case reports (like a COVID‑associated episode) show regrowth once dialysis begins and systemic balance returns .
After a transplant, regaining hair can take 6–12 months, depending on medication regimens. Certain immunosuppressants cause shedding, so adjustments matter.
Key point—hair improvement is contingent on systemic healing. Without addressing anemia, nutrition, medications, or scalp health, shedding may persist. But with proper care, restoration is achievable.
Evidence‑Based Treatments and Management Strategies
Here’s what the research and clinical guidelines suggest for managing kidney‑related hair loss.
1. Collaborative Medical Evaluation
First, your physicians—both nephrologist and dermatologist (or trichologist)—should coordinate. It’s crucial to rule out other causes, confirm lab values (CBC, ferritin, thyroid, vitamin D), and assess medication side effects.
2. Nutritional Optimization
Protein‑energy adequacy must be balanced with dietary restrictions. Specific attention to iron, zinc, selenium, vitamin D—but only under medical guidance. Overdoing supplements (especially vitamin A or E) can backfire in CKD.
Studies highlight that correcting deficiencies can support follicle recovery .
3. Treating Anemia
Providing EPO or iron repletion, when appropriate, restores oxygen delivery to hair follicles. Clinical reviews document regrowth timelines matching anemia correction (~3–6 months).
4. Medication Review
If hair shedding begins after starting beta‑blockers, heparin, or certain immunosuppressants, consult your doctor. A medication tweak may reduce hair loss without compromising renal care.
5. Scalp and Lifestyle Support
Gentle hair care—mild, sulfate‑free shampoo, avoid tight styles, limit heat styling. Manage itching (often via topical emollients or uremic pruritus treatments). And stress—stress management, adequate hydration, and modest protein intake all play a role.
6. Adjunct Therapies
Minoxidil might be considered, especially post‑transplant or in prolonged telogen effluvium recovery phases. But only after systemic factors are under control and under doctor supervision.
Research specifically evaluating minoxidil efficacy in CKD patients is limited but anecdotal reports show improvement.
7. Emerging Therapies and Gaps
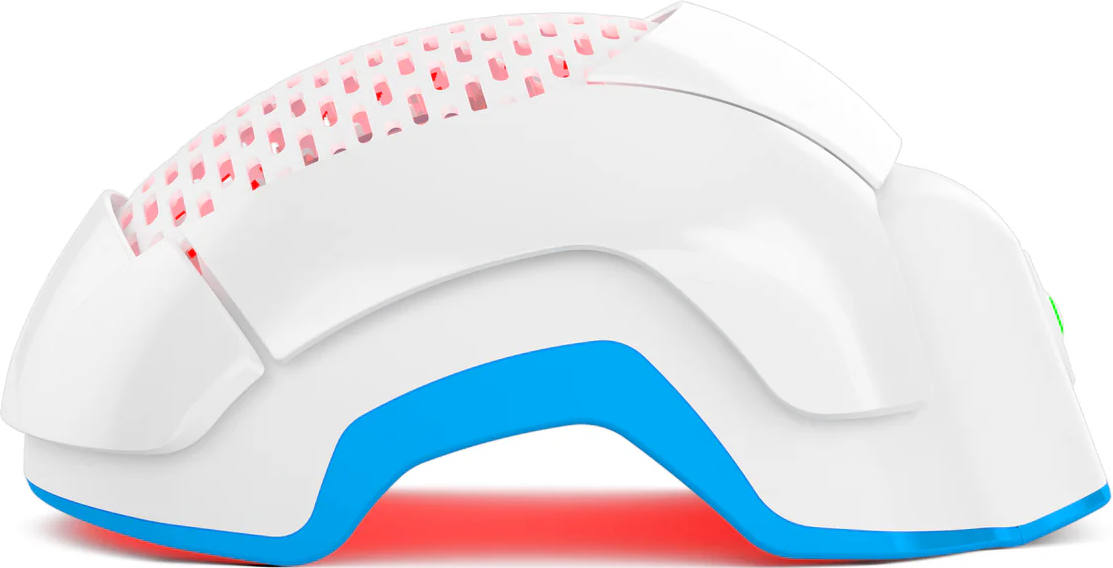
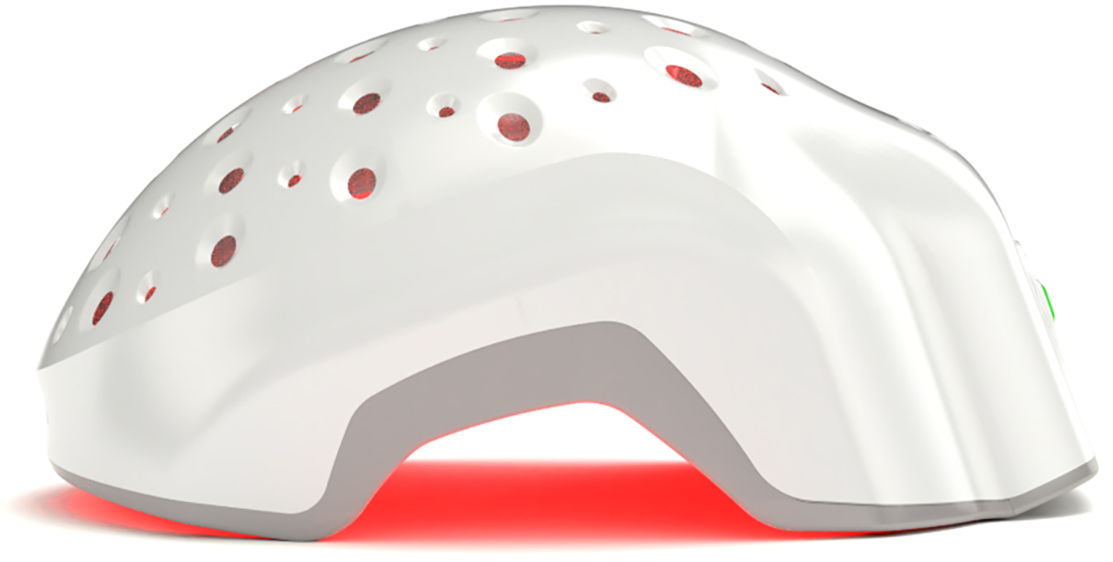
There’s little controlled data on newer treatments like laser‑based scalp therapies (e.g., laser phototherapy/LPT). Anecdotal and theoretical benefit exists—particularly for boosting circulation or improving scalp health.
Recent research is actively examining how photobiomodulation (PBM)—a close cousin of LPT—might benefit people with chronic kidney disease (CKD). A 2022 review highlights PBM’s ability to mitigate mitochondrial dysfunction, quell oxidative stress, soothe inflammation, and even rebalance gut microbiota in CKD models. While no studies have yet directly tracked hair growth outcomes in CKD patients using PBM, this emerging data suggests a plausible link: if PBM helps restore systemic health, it might—and I emphasize might—also pave the way for scalp follicles to recover. Worth future inquiry.
This notion warrants deeper exploration. Imagine investigating whether PBM, which strengthens cellular energy and reduces systemic inflammation in CKD (as shown in the Bian et al. review), might also revive dormant hair follicles weakened by nutrient deficits or oxidative strain. That’s a fascinating hypothesis, right? Especially because CKD often triggers telogen effluvium through interconnected pathways—anemia, hormonal imbalance, toxin buildup. Since PBM improves foundational physiological conditions in CKD, it’s entirely plausible that it could indirectly—but meaningfully—support hair resilience and regrowth. Designing studies that monitor hair parameters (density, thickness, shedding) alongside kidney function markers would be the next step.
Also Read: Future of Laser Phototherapy: The Ultimate Biohacking for Hair Loss
When to Seek Professional Help?
There’s a point (usually when the hair in your brush starts to feel like too much evidence) that waiting it out no longer feels reasonable. If you’ve noticed diffuse shedding for over three months, or your scalp looks thinner in photographs, that’s a quiet nudge to involve a professional. Not just anyone. A dermatologist or trichologist familiar with systemic hair loss patterns and your nephrologist, ideally in tandem.
What’s the red flag moment? Sudden, patchy loss. Or if brittle strands are accompanied by scalp discomfort, severe itching, or new ridges in your nails. (Strange, right? But systemic deficiencies often cluster in these subtle signs.) Sometimes, hair loss is the first outward cry that your labs are shifting—iron or vitamin D dipping, thyroid wobbling.
And don’t self-prescribe supplements. CKD complicates the safety of common remedies. High-dose biotin, for instance, can interfere with lab tests. Unsupervised iron can be dangerous. A specialist can help untangle the overlap between kidney function, medications, and follicle health… which is rarely straightforward.
Conclusion
Hair thinning tied to kidney disease is a peculiar companion… quiet, unsettling, and often overlooked. But in many cases, it’s reversible. Stabilizing lab values, improving nutrition, and (yes) dialing in dialysis or post‑transplant care can allow follicles to wake back up… slowly, stubbornly, but surely.
Does it return overnight? No. Like in seasons, not days. Three to six months for early regrowth, sometimes a year for fullness. And yet, the emotional weight of seeing those first baby hairs is immense relief.
If nothing else, remember that diffuse shedding in CKD is a systemic signal. Listen to it. Partner with your doctors. Maybe even keep a hair diary.
So—strands in the drain aren’t the end of the story. They’re an invitation. With patient care, and occasionally a few gentler shampoos and lifestyle tweaks, your scalp can recover its quiet confidence. And perhaps, somewhere in that slow regrowth, you’ll reclaim a little of yours too.