Hair loss is unnerving. Full stop. Especially when it creeps in quietly—weeks after starting a medication that’s supposed to help you feel better. If you’re taking Wellbutrin (or its generic, bupropion) and you’ve noticed extra strands in your shower drain or a part line that wasn’t quite that wide a month ago… you’re not alone. And no—you’re not crazy.
At its core, Wellbutrin is a brand name for bupropion hydrochloride—a prescription medication for depression categorized as a norepinephrine-dopamine reuptake inhibitor (NDRI). It was originally cleared by the FDA for treating major depressive disorders, and now, millions of individuals rely on Wellbutrin to manage symptoms of depression, anxiety, and even smoking cessation under the name Zyban.
While bupropion works well as an antidepressant, it also has typical side effects such as insomnia, dry mouth, changes in appetite, and hair loss. Let's dive deep into Wellbutrin hair loss.
Does Wellbutrin Cause Hair Loss?
Now for the big question: Does it? Can this seemingly clean, serotonin-free antidepressant cause your hair to fall out?
Short answer: Yes—but it’s rare.
According to a retrospective cohort study published in the International Clinical Psychopharmacology Journal (Etminan et al., 2018), people taking bupropion were 46% more likely to report hair loss compared to those on fluoxetine (aka Prozac). That’s a hazard ratio of 1.46, which sounds clinical and cold until you zoom in: For every 242 people taking bupropion over two years, one additional case of hair loss occurred compared to fluoxetine. Small odds, but not zero.
And that’s not the only signal.
Postmarketing data points to 1–4% of people experiencing telogen effluvium—a type of diffuse hair shedding triggered by internal stressors, including medications. Most cases show up within the first three months of treatment, though some linger longer. But—and this is important—most reverse after stopping or adjusting the dose.
Still skeptical? That’s fair. Let’s check the FDA labeling: “Alopecia” is indeed listed as an uncommon adverse effect, meaning it’s documented in 0.1–1% of users. That may not sound like much, but for the thousands of people prescribed Wellbutrin every month, it’s a number worth respecting.
So, yes. Wellbutrin can cause hair shedding. It’s not common, but not imaginary either.
Why Does Wellbutrin Cause Hair Loss?
So what gives? Why would a drug meant to boost mood and energy quietly sabotage your follicles?
Telogen Effluvium: The Primary Culprit
The best theory—and it’s more than theory, really—is telogen effluvium. This is a condition where hair follicles, spooked by a metabolic or emotional shift (in this case, a medication), prematurely exit the growth phase (anagen) and enter rest mode (telogen). A few weeks later, those hairs shed. Not in clumps, not in dramatic patches—just... more than usual.
How Wellbutrin Affects Your Hair?
Now, here's the rub: Wellbutrin isn’t “toxic” to hair follicles. It doesn’t poison the root or shrivel your scalp. Instead, it may trigger a systemic ripple—a biochemical shift that nudges follicles into hibernation.
- Dopamine Agonism: Some researchers suspect that dopaminergic modulation could play a role in hair cycling. Bupropion's effect on dopamine receptors may disrupt the natural hair cycle. (Though to be blunt, we don’t have a neat mechanistic blueprint for this yet.)
- Stress Response: If you're already battling depression or anxiety, your baseline cortisol may be elevated—priming your follicles for stress-induced shedding. So when you add a new neurochemical agent into the mix, your body's physiological response to starting a new drug, or changes in mood/anxiety, could induce stress that triggers shedding.
- Dose-Dependent Effect: Taking higher doses of Bupropion/Wellbutrin can make hair shedding happen faster and more intensely. This suggests that the amount of medication you take might directly affect how much hair you lose, making careful dosage management important.
Truthfully, there's no single culprit here. Some dermatologists speculate the issue could also stem from indirect hormonal shifts or micronutrient disruptions. But again—most cases are temporary, and the follicles, once nudged back into balance, restart growing hair.
Just... not overnight.
What Does Wellbutrin-Linked Hair Loss Look Like?
It’s not dramatic. That’s the weird part.
Wellbutrin-related hair loss doesn’t usually come in patches like alopecia areata. It’s rarely aggressive or localized. Instead, it’s sneaky—subtle. It’s like a slow fade rather than a harsh chop. What you’ll likely see is diffuse thinning, especially across the crown or along your part line. Your ponytail might feel... lighter. Your brush fills faster. Nothing alarming at first, until—well, it’s something you can’t unsee.
There’s no burning. No itching. No bleeding scalp or tenderness (though if that does happen, talk to a dermatologist ASAP—it’s probably unrelated to the medication).
What falls out? Mostly scalp hair. Body hair, brows, and lashes are typically unaffected, unless there's another issue in play. Some users mention brittle strands or dryness, but that’s more often haircare-related than pharmaceutical. Remember: we’re talking about telogen effluvium here, not follicular destruction. The follicle itself is fine—it’s just... resting. Prematurely.
And timing? If Wellbutrin is the trigger, the shedding tends to begin 1–3 months after starting the medication. Which makes things even murkier, because by that time you’ve often moved past the “Is this causing side effects?” phase and into the “I’m doing better now, finally” one.
That delay makes it harder to spot—and harder to link.
Is It Really Wellbutrin That's Causing Your Hair to Shed?
Hair loss is a tricky narrator. It rarely tells a straight story.
So before blaming Wellbutrin outright (tempting as it is), let’s talk context. Because sometimes—often, actually—the culprit is wearing a disguise.
-
Depression: Depression itself is a well-documented trigger for telogen effluvium. The chronic stress, poor sleep, dietary shifts, even hormonal shifts that accompany a depressive episode? All can contribute to follicle fallout. That alone might be enough to explain the shed.
-
Nutritional Deficiency: Then there’s the issue of nutritional deficiency. Ferritin (your body’s iron storage), vitamin D, zinc—these all impact follicular activity. If your reserves are low, hair loss will often show up as the first sign, not the last.
- Thyroid Issues: Let’s not forget thyroid dysfunction either. Hypothyroidism and hyperthyroidism can both throw off the hair cycle. And if you’re female, there’s a whole hormonal matrix (PCOS, postpartum changes, peri-menopause) that might be happening beneath the radar.
How to Tell If You Have Wellbutrin Hair Loss?
Here’s the good news: the timeline matters. If the hair loss began after starting Wellbutrin and improves (or halts) when it’s stopped or adjusted, that’s a clue. But it’s not definitive. It could still be coincidence. Or convergence.
That’s why we don’t jump to conclusions. We track patterns, ask questions, and—ideally—get professional input.
One more thing: If you’ve been on other antidepressants before (say, sertraline or escitalopram), and never noticed hair shedding, that also gives some comparative insight. In clinical studies, bupropion was found to have a slightly higher risk of hair loss than SSRIs. So... yeah. The dots might be starting to connect.
Just don’t connect them too fast.
Here’s how to get clarity without spiraling.
- Start with a timeline log. Seriously—track the dates: when you started Wellbutrin, when the shedding began, any dose changes, any stressful events, dietary shifts, illnesses, hormone fluctuations. The more detailed, the better. (Even if it feels slightly neurotic. Trust your data.)
- Next: bring it to your healthcare team. And not just one doctor. A psychiatrist will understand the drug. A trichologist or dermatologist understands the scalp. Ideally, they talk to each other (but let’s be honest, they rarely do).
They might run:
- Blood work (CBC, ferritin, thyroid panel, vitamin D, etc.)
- Scalp exam (visual inspection, dermoscopy)
- Hair pull test (gentle tug to assess shedding)
- Possibly a biopsy (rarely, but it’s a thing)
But even without invasive testing, a good clinician can spot telogen effluvium by pattern and timeline. It’s distinctive. And yes—many will have seen this exact scenario before.
Is Wellbutrin Hair Loss Permanent?
Wellbutrin-related hair loss is rare, and when it happens, it’s usually temporary. The majority of people notice regrowth once their dosage is adjusted or after their body adapts to the medication. In many cases, hair shedding slows down or stops entirely within a few weeks of starting treatment.
Now, let’s be clear. Everyone’s body chemistry reacts differently. Some may see a quick recovery; others might need a bit more time. But permanent hair loss from bupropion (Wellbutrin)? That’s not the norm.
If you’re noticing unusual thinning or excessive shedding, don’t panic, and definitely don’t stop taking your antidepressant immediately. Talk to your healthcare provider first. They can help you explore options like dose adjustments, switching medications, or integrating hair regrowth treatments to support your scalp health.
How to Stop Wellbutrin-Linked Hair Loss?
Let’s start here: don’t stop taking Wellbutrin without medical supervision. Seriously. Even if your hair’s falling out like autumn leaves on fast-forward. Abrupt withdrawal can lead to mood crashes, agitation, and even withdrawal-like symptoms in some people. Your brain chemistry deserves respect. Always speak to your prescribing doctor first.
Now, adjusting your dosage might help. Some patients report that lower doses slow the shedding. The goal isn’t panic; it’s partnership—with your doctor, with yourself.
If medication change is on the table, some prescribers suggest trying another antidepressant class. SSRIs like sertraline or escitalopram are generally considered to have a lower hair-loss risk than bupropion. But again: mental health comes first. Always.
Okay... so what if you can’t change meds? Or you don’t want to?
That’s where supportive therapies step in.
Here’s how to manage Wellbutrin-induced hair loss, practically and calmly:
- Talk to Your Healthcare Provider: If you’re worried about hair loss, bring it up with your doctor. They can help determine whether Wellbutrin is the cause and what adjustments might make sense for you.
- Nutritional Support: Your hair reflects what’s happening beneath the surface. Focus on a balanced diet packed with biotin, iron, zinc, and protein—nutrients that help fuel healthy hair growth. Eat eggs, leafy greens, salmon, and nuts.
- Gentle Hair Care Practices: Skip harsh products and switch to gentle, sulfate-free shampoos and conditioners. Go easy on heat tools and tight hairstyles that can cause breakage.
- Manage Your Stress: Stress can accelerate shedding. Try meditation, yoga, or even short daily breathing breaks to help your body and mind reset.
- Regular Scalp Massage: Gently massage your scalp regularly. This helps to improve blood circulation to your scalp and hair follicles, and also reduces cortisol for stress management.
- Take Hair Supplements: Some people find that biotin or hair-growth supplements make a difference. Just don’t self-prescribe. Check with your healthcare provider first to make sure they fit your needs.
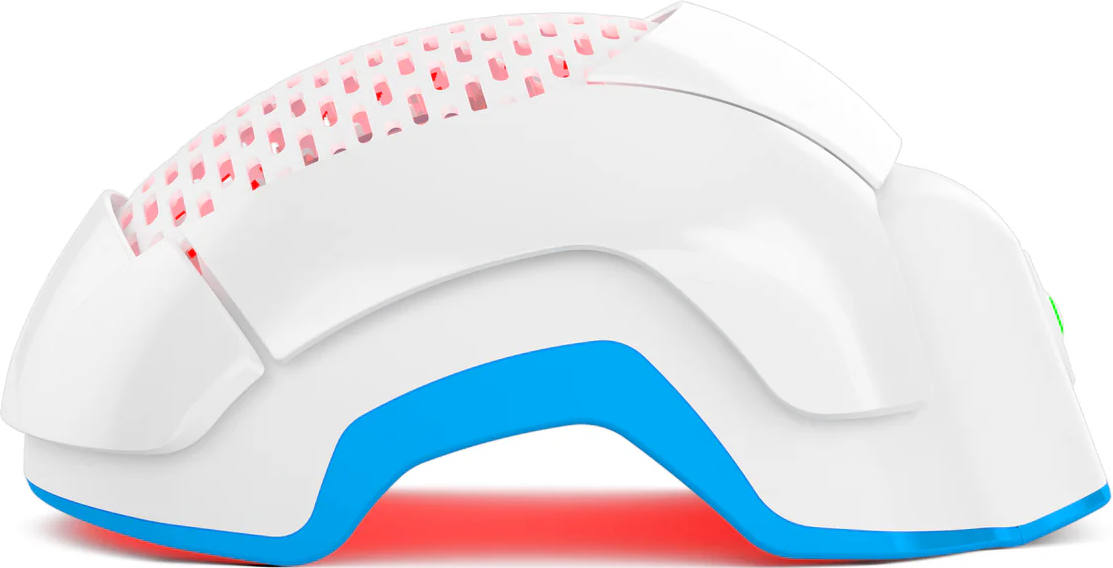
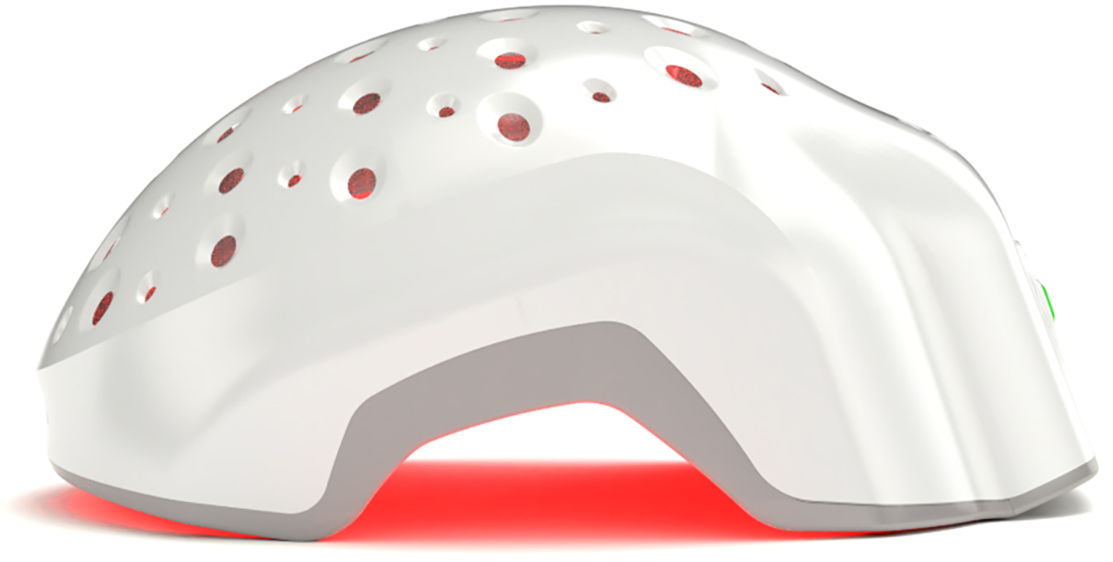
- Consider Laser Phototherapy: This is where science steps in. Low-Level Laser Therapy (LLLT)—also known as laser phototherapy—is an FDA-cleared, non-invasive treatment that helps stimulate dormant hair follicles and boost blood flow to the scalp. Over time, this can encourage thicker, healthier hair growth. Devices like Theradome’s laser hair growth helmets use this technology to deliver consistent, clinic-grade results from home—without drugs or side effects.
Conclusion
If you made it this far—you’re not just curious. You’re concerned. Maybe frustrated. Probably tired of Googling this in the middle of the night when your scalp feels too... visible.
Let’s leave you with this:
Yes, Wellbutrin can cause hair loss.
No, it’s not common.
Yes, it’s usually reversible.
And yes, your mental health still matters most.
But so does how you feel in your skin. On your head. In the silence between doctor visits.
So don’t ignore it. Don’t downplay it.
Track it. Talk about it. Treat it if needed.
And if it’s helpful to hear—most people who deal with this do get their hair back.
Sometimes slowly. Sometimes stubbornly. But it happens.
There’s space for both: healing your mind, and protecting your hair.
You’re allowed to want both.