Androgenetic alopecia (AGA) is a hereditary, androgen-driven condition where susceptible scalp hair follicles gradually shrink (miniaturize), leading to characteristic thinning in men and women. Early diagnosis and scientifically supported treatments (like minoxidil, finasteride where appropriate, and Laser Phototherapy [LPT]) often slow or reverse loss—but starting later means slower or weaker results.
What Is Androgenetic Alopecia?
Androgenetic alopecia (often called male-pattern baldness or female pattern hair loss) is the most common non-scarring hair loss in adults. It involves a hormonal and genetic interplay that causes scalp hair follicles to miniaturize (become thinner and shorter) over time.
Men typically show receding hairlines and baldness on the top (“vertex”) of the scalp. Women usually experience diffuse thinning, especially over the crown and central line, often without a receding frontal hairline.
It begins subtly (often in late teens to early 20s for men, later onset for women), progresses gradually, and without treatment can lead to significant thinning. Internal scalp mechanisms (androgens, genetics, follicle sensitivity) drive this process.
How Do Signs Differ in Men and Women?
Androgenetic alopecia (AGA) is by far the most common form of hair loss—accounting for roughly 93% of all hair loss conditions reported globally. It doesn’t discriminate. It affects up to 50% of both men and women, though how it manifests can differ widely. By the age of seventy, around 80% of men will show some degree of AGA. For women, the likelihood rises sharply after menopause, as hormonal changes amplify follicular sensitivity to androgens.
The emotional and psychological effects are often underestimated. Some people notice it subtly (thinner ponytails, wider parts) while others see clear recession or thinning patches. Yet, whatever the presentation, the biological engine remains the same: inherited follicular sensitivity to androgens like dihydrotestosterone (DHT).
Early warning signs in men
- Receding temporal hairline (“M-shape”) is common.
- Thinning at the crown (vertex) often appears next.
- Hair may appear densest on sides/back, less on top.
- Hair becomes finer and shorter before falling out (miniaturization).
Early warning signs in women
- Wider mid-scalp part, especially above crown.
- Diffuse crown thinning rather than distinct bald spots.
- Less likely to have frontal recession; more likely noticeable overall scalp thinning.
Clinical classification systems
- Hamilton-Norwood scale (for men): stages I through VII; helps standardize description of the pattern.
- Ludwig scale (for women): three main grades based on crown thinning.
These help in diagnosis and tracking treatment outcome.
What Causes Androgenetic Alopecia?
Dihydrotestosterone (DHT), produced by 5-alpha reductase converting testosterone, binds to androgen receptors in scalp follicles. In those genetically susceptible, it shortens the growth (anagen) phase and lengthens rest (telogen), gradually shrinking follicles. This miniaturization reduces hair diameter and length.
Genetics and family history
- Variants in the AR gene (on X chromosome) are strongly implicated.
- Multiple other genetic loci from genome-wide association studies add risk (polygenic inheritance).
- Family history matters: both maternal and paternal lines—but AR gene means maternal lineage is often emphasized.
Hormonal influences
- Conditions with androgen excess (e.g. PCOS in women) may accelerate thinning.
- Menopause alters estrogen/testosterone balance, increasing effective androgen exposure in scalp.
- Andropause (age-related decline in testosterone, but sometimes imbalance) may contribute in men.
Environmental & lifestyle factors
- Smoking has been associated with earlier or more severe AGA.
- Metabolic syndrome, insulin resistance may correlate.
- Poor scalp care / chronic inflammation could aggravate.
- Diet, stress, sleep—supportive roles, not primary causative except in extremes.
How Is Androgenetic Alopecia Diagnosed?
- Begin with patient history: onset, pattern, family history, medications, lifestyle.
-
Physical examination: pattern of thinning, scalp condition, shedding vs miniaturization.
Trichoscopy (dermoscopic examination)
- Trichoscopic features that strongly suggest AGA include:
- Hair diameter variability in ~94% of patients.
- Increased number of vellus hairs (fine, thin non-pigmented) in ~66%.
- Peripilar sign (brownish halo around follicles) in ~43% in certain studies.
These are high-yield features, especially when comparing frontal vs occipital scalp.
When labs & further tests are needed
- If signs point elsewhere: rapid shedding, patchy loss, scalp symptoms (itching, burning).
- Blood tests: thyroid panel, iron studies, maybe androgen levels in women.
- Laboratory studies are mainly to rule out rather than diagnose AGA.
What Treatments Actually Work?
FDA-approved frontline treatments
- Topical minoxidil: 2% and 5% formulations. The 5% tends to work faster and stronger in men; in women the difference is more modest. FDA-approved; requires continuous use—ceasing leads to regression to prior state.
- Finasteride 1 mg/day (men): inhibits 5-alpha reductase type II, lowers DHT, slows progression, often leads to regrowth especially at vertex. Cannot be used in pregnant women and women of childbearing potential. Side effects include sexual dysfunction for some, mood effects under investigation.
Low-dose oral minoxidil (off-label)
- Used in lower doses (0.25-5 mg/day) when topical application insufficient or poorly tolerated. Studies suggest efficacy in both sexes.
- Side effects: hypertrichosis (unwanted hair), blood pressure changes, etc. Must be monitored.
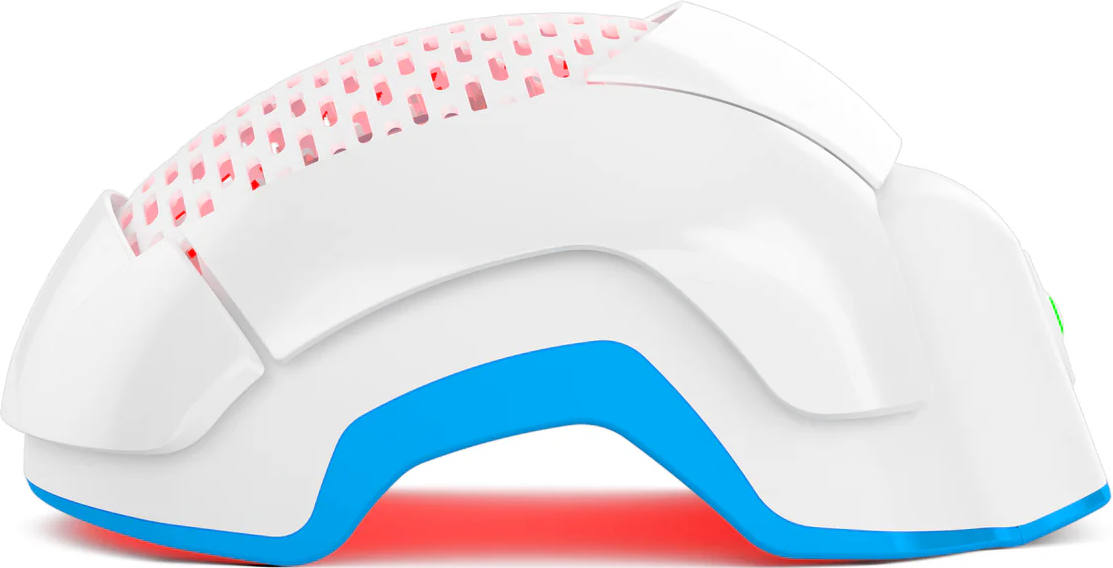
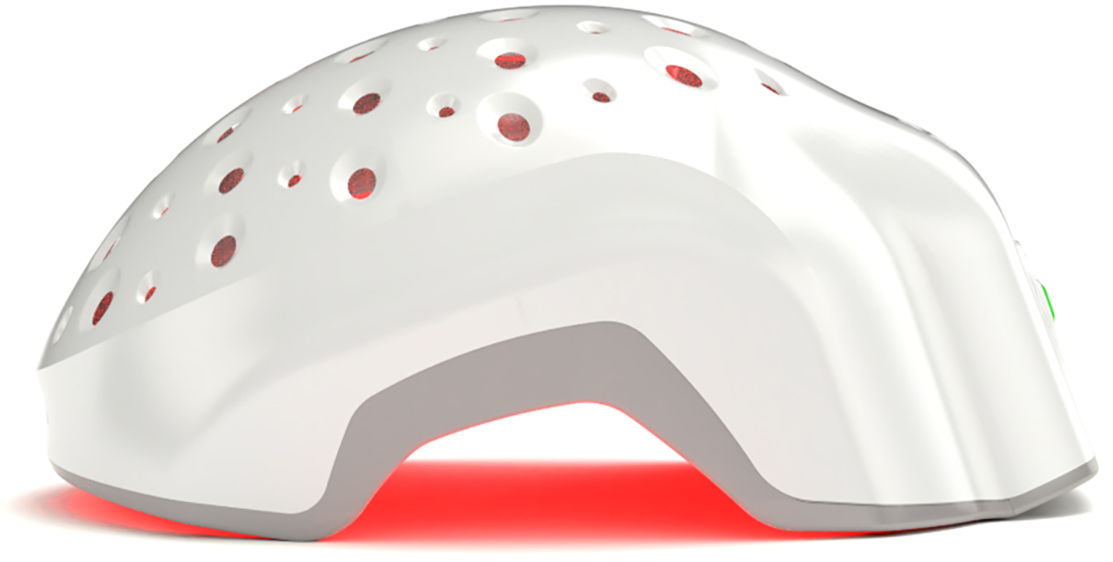
Device-based therapies: Laser Phototherapy (LPT)
Over the past decade, Laser Phototherapy (LPT) has evolved from experimental to evidence-backed adjunct therapy for androgenetic alopecia. Multiple randomized clinical trials (RCTs) and systematic reviews confirm its safety and efficacy for both male and female pattern hair loss.
A systematic review by Gentile & Garcovich (2021) analyzed 298 publications, narrowing to 36 LPT-focused studies, of which seven were RCTs. All RCTs reported positive effects on hair density or thickness in male and female participants, with no significant side effects reported (Facial Plast Surg Aesthet Med, 2021).
Similarly, Gupta & Foley (2017) performed a critical evidence review of low-level laser therapy in Dermatologic Surgery and found consistent clinical improvement across trials, reinforcing that properly calibrated red-light devices (600–950 nm) can stimulate follicular growth through photobiomodulation without thermal damage (Dermatol Surg, 2017).
In another comprehensive literature review, Egger et al. (2020) summarized ten RCTs, eight of which compared LPT devices to sham treatments. Every sham-controlled study demonstrated statistically significant increases in hair diameter and density (p < 0.01) following treatment (Skin Appendage Disord, 2020).
Specific helmet-type devices—like those studied by Yoon et al. (2020) in Medicine (Baltimore)—produced significant hair-density gains after 16 weeks of twice-weekly sessions (Medicine (Baltimore), 2020).
Of particular note, Theradome PRO LH80, an FDA-cleared LPT helmet, was evaluated in a multicenter, double-blind, sham-controlled trial (Gold et al., NCT02528552). Results showed that its 680 nm wavelength penetrates the scalp approximately 2.5× deeper than the 630–655 nm range used by most consumer devices—translating to improved absorption and faster biological stimulation. Participants achieved visible benefits after twice-weekly 20-minute sessions, compared to the daily or near-daily frequency typically required by less powerful devices.
Earlier foundational work by Lanzafame et al. (2013, 2014) found that both men and women using red-light helmets experienced 30–37% greater hair regrowth versus placebo after just 16 weeks of consistent use, with no reported adverse effects (Lasers Surg Med 2013; Lasers Surg Med 2014).
When combined with topical minoxidil, several studies observed an accelerated onset of regrowth and enhanced density compared to either therapy alone (Karger, 2021).
LPT is a clinically validated, low-risk adjunct for androgenetic alopecia. Cold-laser helmets (especially FDA-cleared, medical-grade devices like Theradome) offer consistent safety and measurable results for both sexes. The cumulative evidence from RCTs, meta-analyses, and systematic reviews underscores that LPT enhances follicular activity, increases hair density, and improves overall scalp health without the side effects linked to pharmacologic agents.
Procedural or adjunctive treatments
- Platelet-rich plasma (PRP): meta-analyses show improved hair density vs placebo in 3-6 month periods; outcomes depend heavily on protocol (number of injections, volume, frequency). Some downside: cost, variable results.
- Microneedling: when combined with minoxidil, better results than minoxidil alone in some trials. Wiley Online Library
- Hair transplantation (FUT / FUE): for those with stable donor areas; surgery transfers healthy follicles from sides/back to thinning regions. Good for more advanced thinning but invasive, costs, recovery, realistic expectations are vital.
Combination strategies
Meta-analyses show combining treatments (minoxidil + finasteride; minoxidil + LPT; etc.) yields superior outcomes over single modality.
But more side effects, greater burden must be weighed. Patient goals, tolerance matter.
How Long Until Results Show, and Will They Last?
- Visible improvements often begin around 3-4 months into treatment (for minoxidil / LPT), with more substantial changes by 6 months or more.
-
For finasteride, data shows benefits continuing over years; stopping often results in return toward baseline.
- Duration and maintenance: most treatments require long-term or indefinite use. Expect variance: early vs late stage responses differ.
Can Lifestyle and Scalp Care Slow AGA?
- Smoking is associated with increased severity and earlier onset in men in several observational studies. Eliminating smoking may slow progression.
- Metabolic health (insulin resistance, obesity) correlated with worse outcomes; addressing diet, exercise, sleep helps scalp environment even if it doesn’t reverse strong genetic drive.
- Scalp hygiene: reducing chronic inflammation, avoiding harsh chemicals helps support treatments.
- Nutrition: ensure adequate protein, iron, vitamin D—but unless deficiency confirmed, supplements are supportive not curative.
Psychological and Social Impact of AGA
- Many people with AGA report reduced self-esteem, social anxiety, stress. The burden often greater in women due to diffuse thinning patterns.
- Treatment outcomes sometimes insufficient to match expectations; managing expectations is a critical part of clinical care.
- Support: counseling, peer groups, influencing lifestyle etc. are part of holistic management.
When Should You See a Trichologist or Dermatologist?
- If hair loss is rapid, patchy, or accompanied by scalp symptoms (itching, burning).
- If over-the-counter or home treatments not helping after ~3-6 months.
- If you want a professional diagnosis (trichoscopy), treatment plan, sometimes procedural options.
- Bring: photos (onset, previous state), any lab results, medications, relevant family history.
Conclusion
Androgenetic alopecia is not an automatic sentence. With proper diagnosis and an evidence-based plan (often combining treatments, using LPT adjuncts, and sustaining therapy), many people see meaningful improvement. You may not get every hair back—but slowing loss, improving density, and boosting confidence are very achievable goals. Stay engaged with a trained clinician, adjust as needed, and don’t give up early—sometimes the slow gains are the ones that last.