Tinea capitis is a fungal infection of the scalp and hair shafts (commonly called “scalp ringworm”). It causes patches of hair loss, scaling, itching — and must be treated with oral antifungals; topical creams alone won’t cut it.
What Exactly Is Tinea Capitis?
Tinea capitis is literally just a fungal infection of the scalp. "Tinea" means fungal (specifically dermatophyte-related), and "capitis" means… well, your head.
So what we’re dealing with here is scalp ringworm — not an actual worm, but a keratin-loving fungus that thrives in hair shafts and skin folds, particularly the kind that stay warm, slightly damp, and covered for too long. (Looking at you, hoodie-all-day people.)
But why does it like the scalp so much?
Why fungus targets the scalp
The scalp, it turns out, is like beachfront property for certain fungi — warm, humid, a little oily, and often wrapped in hats, wigs, bonnets, or scarves that trap heat like a Dutch oven. It’s literally the hottest part of the human body in terms of surface temperature. (Which is why every mom checks your forehead for a fever, not your elbow.)
Now add hair (which naturally holds heat and moisture) and we’ve got the kind of microclimate fungi adore.
According to research, the higher the scalp temperature, the more likely fungal overgrowth becomes. And in those genetically predisposed to MF sensitivity (that’s Malassezia furfur, a yeast-like fungus), the result can trigger inflammatory responses, itching, and even hair loss. All just from heat, moisture, and a few tight head coverings too many.
Oh — and yes, this explains why:
- Athlete’s foot
- Jock itch
- Under-breast fungal rash
- and scalp ringworm
...all have eerily similar causes: warm, damp, covered environments.
So when dermatophytes like Trichophyton or Microsporum get involved (especially in the scalp of a child, where oil composition is different and immune barriers less robust), they find the perfect breeding ground. They slip into the hair shaft, disrupt the follicle, and cause patchy baldness, flaking, sometimes swelling (we’ll get to kerion), and a whole lot of scratching.
Who Gets It—and Why?
Children, Adults, and the Immunity Factor
Most cases occur in prepubescent children, whose scalp environments favor fungal colonization more than post‑pubertal scalps.
But adults aren’t immune — immune suppression, close contact, or untreated infections in the household can make them susceptible.
Transmission & Spread
It spreads via:
- Direct scalp‑to‑scalp contact (hug, close play)
- Shared items: combs, hats, pillows, helmets
- Animal sources (for Microsporum infections)
- Asymptomatic carriers (people or pets may carry spores without visible symptoms)
Spores can survive off-host for days on fabrics, making fomite transmission real.
What It Looks and Feels Like
Common Signs
- Circular or oval patches of hair loss
- Scaling, flakiness, sometimes mild redness
- Broken hairs leaving “black dots”
- Itchiness
- Swollen lymph nodes behind ears or neck
The Inflammatory Type — Kerion
Sometimes the infection triggers an aggressive immune response → kerion. That’s a boggy, tender, swollen plaque that may ooze or discharge. High risk of scarring if not treated early. (Kerion is often misdiagnosed as bacterial abscess).
Conditions It Can Resemble
- Dandruff or seborrheic dermatitis
-
Psoriasis
-
Alopecia areata (autoimmune patchy hair loss)
-
Folliculitis, bacterial infection
Hence the need for diagnostic confirmation.
How Dermatologists Diagnose It
Visual and Clinical Clues
Patterns of hair breakage, scaling, hair loss with classic patches. “Black dot” patches or “gray patch” may suggest tinea.
Confirmatory Tests
- KOH (potassium hydroxide) microscopy of plucked hair — looks for fungal hyphae
- Fungal culture (slow but species identifying)
- Wood’s lamp: some Microsporum species fluoresce green (but Trichophyton usually does not)
- Trichoscopy (dermoscopy of hair/scalp): patterns like comma hairs, corkscrews, black dots help support diagnosis
Why Self‑Diagnosis Can Fail
Visual similarity with other scalp disorders makes guesswork risky. Wrong treatment delays cure, allows spread, increases scarring risk.
Treatment: What Actually Works
Dealing with hair loss or an itchy, flaky scalp messes with your confidence, your mood, even how you show up in your day. And if you’ve tried product after product, advice from random forums, or your auntie's “miracle oil,” it’s easy to feel like everything’s a scam.
But some stuff does work. Not because it’s trendy, but because it’s been studied, tested, and it has the receipts to prove it. We're talking about medicated antifungal shampoos — specifically three ingredients that actually pull their weight: Piroctone Olamine, Ketoconazole, and Zinc Pyrithione.
Let’s break them down. Just what the science says and what real-world results have shown.
Piroctone Olamine (PO)
-
Best for: Hair loss, dandruff, sebum control
-
Found in: Prescription and OTC antifungal shampoos
-
Recommended concentration: 1%
This one doesn’t get the same spotlight as the others, but don’t let that fool you. Piroctone Olamine is quietly one of the best antifungal ingredients for scalp health and hair regrowth. It works by disrupting Malassezia furfur, the yeast responsible for dandruff and inflammation on the scalp. And once inflammation is down, hair follicles are no longer under siege.
Here’s what the research says:
- Hair shaft diameter increased by 7.7%
- Hair loss reduced by 16.5%
- Helps with seborrheic dermatitis, scalp itch, and flaking
- Reduces scalp oiliness by dialing down sebum production
Also important: PO doesn’t come with the same level of irritation or hormonal interference that some other ingredients might carry. It’s tolerated well and plays nicely alongside things like LPT devices, which rely on a calm, inflammation-free scalp to work effectively.
Ketoconazole (Keto)
-
Best for: Dandruff, scalp oil, inflammation, hormone-sensitive hair loss
-
Found in: Prescription and OTC shampoos (e.g., Nizoral®)
-
Recommended concentration: 1–2%
Now we’re in big league territory. Ketoconazole has been widely used for both dandruff and androgenetic alopecia. It’s antifungal, yes — but it also reduces inflammation, cuts oiliness, and even influences hormonal pathways linked to hair loss.
Clinical trials have shown:
- Hair shaft diameter increased by 5.4%
- Hair loss decreased by 17.3%
- Sebum output reduced, which keeps the scalp less greasy and more balanced
- Hair shedding in 24 hours dropped significantly
- Growth-phase hair (a.k.a. the good kind) increased by 6.4%
Some studies even show ketoconazole performs nearly as well as minoxidil in terms of hair density improvements. But it’s not all roses — higher concentrations or overuse can dry out the scalp, cause irritation, or mess with hair texture. Use it wisely.
Zinc Pyrithione (ZP)
-
Best for: Mild dandruff, inflammation
-
Found in: Most over-the-counter anti-dandruff shampoos
-
Recommended concentration: ~1%
You’ve probably used this ingredient without even realizing it — it’s the star in products like Head & Shoulders. Zinc Pyrithione fights yeast and inflammation, which helps keep the scalp balanced. It’s not as powerful as PO or Keto in reversing hair loss, but it holds its own.
What it does:
- Reduces hair loss by 10.1%
- Decreases shedding by 6.02%
- Increases growth-phase hairs by 8.4%
- Doesn't really affect sebum production, unlike the other two
It’s more of a maintenance player. Useful in keeping scalp conditions in check, but probably not enough on its own if you're dealing with aggressive hair loss.
So... Which One Should You Use?
If your goal is healthy, thicker, stronger hair then Piroctone Olamine (1%) is the front-runner. It's shown stronger hair regrowth potential, fewer side effects, and is a smart long-term addition to any scalp health regimen. It also plays nicely with LPT devices by reducing inflammation, which opens up the scalp to respond better to light therapy.
Ketoconazole works great too, especially if you’re dealing with significant sebum, scalp irritation, or hormonally influenced hair loss. Just don’t overuse it, and go for the 1% version unless your practitioner recommends otherwise.
Zinc Pyrithione is decent (particularly for keeping the scalp calm between stronger treatments) but not a stand-alone solution for reversing hair loss.
A Word on Consistency
One-off use won’t cut it. Malassezia doesn’t just disappear; it resurfaces in a matter of days if you stop treatment. This is why antifungal shampoos are often used long-term — not because you’re “addicted” to them, but because you’re keeping fungal populations in check so they don’t set your scalp on fire.
If you’ve had a hair transplant or you’re using a device like LPT, these antifungals are even more essential. A calm, clean scalp is fertile ground. Literally.
Any Downsides?
Yes — even the good stuff comes with fine print.
- Scalp irritation (especially if used too frequently)
- Dryness or oiliness, depending on your skin type
- Possible discoloration of hair in rare cases
- Changes in texture
That said, these effects are usually mild and can be managed with proper usage, spacing out applications, and not combining five different harsh treatments at once.
The antifungal route (especially with piroctone olamine or ketoconazole) is one of the best-supported, evidence-based approaches for improving scalp health and slowing (or even reversing) certain types of hair loss.
Prevention and Hygiene
At Home
- Don’t share hair tools, hats, pillows.
- Wash bedding, towels, pillowcases frequently (hot cycle).
- Disinfect or discard contaminated combs.
- For Microsporum infections, evaluate pets (vet consultation).
In Community Settings
- Inform schools or daycare when a child is infected.
- Limit close contact until antifungal therapy begins.
- Use medicated shampoo on family members as preventive measure (twice weekly for some weeks).
Recovery and Hair Regrowth
What to Expect Post‑Treatment
- Hair regrowth can be slow; some shedding continues as follicles recover.
- Areas with scarring (often from kerion) may not fully regrow.
- Full cosmetic recovery may take months or longer.
Supporting Scalp Health
- Gentle shampooing, avoid harsh chemicals or tight styles.
- Balanced nutrition, scalp microcirculation, rest.
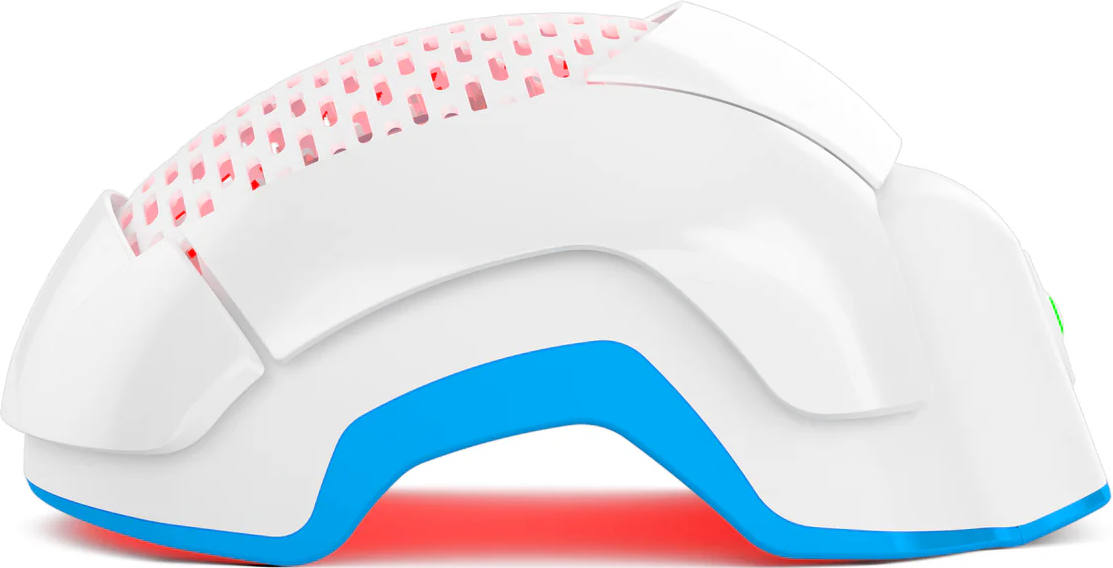
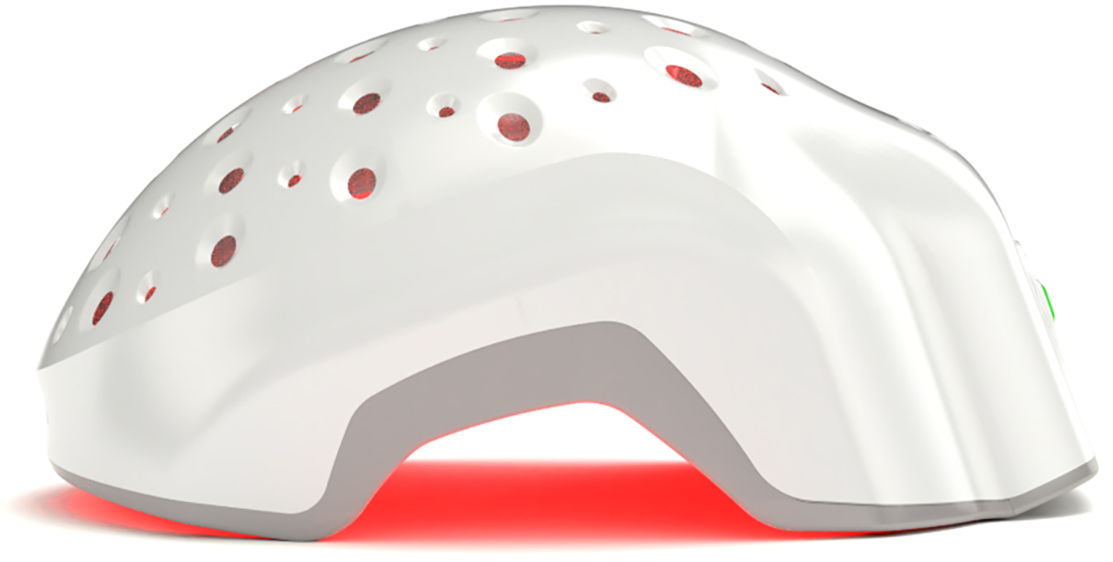
Role of Laser Phototherapy (LPT) — After Infection Clears
- Important caveat: LPT is not a substitute for antifungal treatment during active infection.
- After clearance, low-level lasers (aka photobiomodulation) may stimulate mitochondrial activity, increase microcirculation, reduce inflammation, thus helping follicles regain vigor.
- Meta‑analyses of FDA-cleared devices show statistically significant increases in hair density vs sham in androgenetic alopecia settings (SMD ≈ 1.27).
- Safety profile is favorable across trials, minor side effects such as scalp mild irritation reported.
- It’s a supportive, regenerative tool, not antifungal therapy.
When to See a Specialist
- Rapidly enlarging swelling or pain (possible kerion)
- Pus, crusting, or systemic symptoms (fever)
- Lack of improvement after 2 weeks of therapy
- Hair loss continues or scarring observed
- Emotional distress over visible patches
Specialists (dermatologists/trichologists) can refine diagnosis, culture for species, tailor therapy, monitor complications.
Conclusion
Tinea capitis is treatable — but it demands correct identification and a full course of oral antifungals. If you catch it early, scarring is preventable and regrowth is very likely. After medicine clears the infection, gentle care and regenerative tools like Laser Phototherapy can help coax your follicles back toward strength.
Take care of the scalp, don’t skip doses, and consult a specialist if things don’t improve. Your follicles deserve the chance — light, vigilance, and consistency make a difference.