A medical device worn directly on your head demands the strictest possible manufacturing ecosystem… and in the United States, FDA-regulated quality systems, traceability laws, and engineering controls create a level of safety and consistency that offshore production simply cannot match.
There’s something quietly primal about the human head. People will expose their elbows to the world, shrug off a bruise on a knee, laugh about a paper cut… but when something approaches the scalp — the thin stretch of skin protecting the brain, the delicate follicular microenvironment, the optic pathways that translate light into sight — the instinct shifts. You guard your head differently. You judge risk differently.
So when someone places a laser medical device on that territory, the question isn’t simply whether it “works.”
It’s whether the engineering behind every photon, every component, every calibration step, follows a manufacturing ecosystem that treats this proximity with the seriousness it deserves.
This is where “Made in the USA” becomes a framework of protection.
Because for medical devices (especially Laser Phototherapy (LPT) systems used for androgenetic alopecia) manufacturing origin affects:
- safety
- optical stability
- dose accuracy
- durability
- regulatory accountability
- and ultimately… clinical outcomes
What Does “Made in the USA” Actually Mean?
It’s tempting to view the phrase as a marketing flourish, something splashed on packaging to evoke trust or patriotism… but in reality, “Made in the USA” is a legally regulated claim overseen by the Federal Trade Commission (FTC). And unlike many countries, the U.S. enforces this label with the kind of precision you’d hope for in medical technology.
According to the FTC’s Made in USA Labeling Rule, a product must be “all or virtually all made in the United States.”
Not assembled.
Not designed.
Not partially sourced.
All or virtually all.
That means the final assembly, significant processing, and primary components must originate domestically. If a company violates this rule, the FTC can impose serious civil penalties. Williams-Sonoma learned this the hard way when they paid over $3 million for falsely labeling imported goods as U.S.-made.
For a consumer choosing something worn directly on their scalp (a zone just millimeters from cranial bone and neural pathways), this matters more than people think. “Made in the USA” becomes a shorthand for:
- traceable suppliers
- stricter material controls
- documented design history
- enforced safety validation
- accountable manufacturers
In other words, you know who built it, under which rules, and with what oversight.
That level of clarity is uncommon globally, particularly in high-volume offshore manufacturing ecosystems where supply chains sprawl, subcontractors multiply, and accountability thins out.
But in the United States, traceability is baked into the regulatory spine.
How Do U.S. Manufacturing Standards Protect You?
For medical devices (including Laser Phototherapy (LPT) helmets for hair regrowth), the United States enforces one of the most stringent and intrusive quality frameworks on the planet. And it’s about to become even stronger.
FDA QSR → QMSR (2026) & ISO 13485 Alignment
Right now, all U.S. device manufacturers must comply with the FDA Quality System Regulation (QSR; 21 CFR Part 820), which governs:
- design controls
- supplier qualification
- process validation
- complaint handling
- device history records
- auditing
- change management
You can find the details of this system given by FDA here.
But in 2026, the U.S. moves into a new era: the Quality Management System Regulation (QMSR) — a rule fully harmonized with ISO 13485:2016, the global medical device standard.
You can check the Final Rule published in Federal Register of US Government.
What does that mean for consumers?
1. Stronger Design Documentation
Every optical component, wavelength, irradiance calibration, and laser parameter must be documented and auditable.
2. Stronger Supplier Oversight
Components must be verified, validated, and traceable. No anonymous part substitutions.
3. Stronger Post-Market Surveillance
Manufacturers must track device behavior in the real world and correct issues proactively.
4. Stronger Alignment with Global Standards
ISO 13485 principles (risk management, sterile barrier integrity, calibration control) become U.S. law.
It is worth noting:
ISO 13485 certification alone does not exempt a company from FDA scrutiny.
The FDA explicitly states that while the QMSR aligns with ISO 13485, manufacturers are still fully subject to FDA inspections.
This dual-layer oversight is rare worldwide and provides something offshore systems often lack:
Predictability. Consistency. Accountability.
Because with U.S. manufacturing, a medical device isn’t simply built.
It’s continuously verified.
Safety and Consistency in Laser Devices
Laser Phototherapy (LPT) is not warm light, not LED glow, not a “red-light gadget.” LPT uses precisely tuned coherent light, and the safety of that light is governed by:
- IEC 60825-1 (international laser safety standard)
- FDA Laser Notice No. 56 (U.S. adoption of key IEC elements)
LPT devices for hair growth typically operate as Class 3R “cold” lasers — meaning they do not heat tissue, but they do penetrate to interact with mitochondrial chromophores.
But here’s the critical truth almost no brand explains:
Laser therapy is only safe and effective when the optical output is stable.
If optics drift…
If alignment shifts…
If divergence increases…
If wavelength tolerances wander outside the therapeutic range…
Then the biological effect collapses.
Poor manufacturing can cause:
- inconsistent wavelength
- unstable irradiance
- hotspots
- excessive scatter
- power drift over time
All of which directly determine whether the follicle receives:
- a therapeutic dose,
- an ineffective dose,
- or (rarely) an excessive one.
This is why U.S. manufacturing controls matter.
The precision required for LPT thrives in a strict regulatory ecosystem, and it falters in a loose one.
Why Precision Is Critical in Laser Phototherapy (LPT)
If there’s one idea consumers rarely hear (and absolutely should), it’s this:
Laser Phototherapy is not “red light.” It is bioenergetic signaling.
Your hair follicles aren’t responding to brightness, warmth, color, or ambiance.
They respond to photons of a very specific wavelength, delivered at a very specific irradiance, for a very specific duration, via an optical system that must stay stable across thousands of cycles.
The biological mechanism sits primarily in the mitochondria.
When photons in the therapeutic range (often around 650–680 nm or 785–808 nm, depending on the device design) reach the follicular bulge and dermal papilla, they interact with:
- Cytochrome c oxidase (a key enzyme in the respiratory chain)
- Nitric oxide (NO) modulation
- ATP upregulation
- Reactive oxygen species (ROS) signaling
- Transcription factor activation
Here’s what quietly defines the entire LPT field:
The biphasic dose response.
Too little → nothing happens.
Too much → biological inhibition.
Too inconsistent → unpredictable results.
This is called the Arndt–Schulz curve, and it is the biochemical reason manufacturing origin matters more for LPT than for many other consumer devices.
Because in an LPT system:
- wavelength drift = wrong chromophore absorption
- irradiance instability = wrong mitochondrial stimulation
- optical misalignment = patchy scalp coverage
- component variance = inconsistent results across users
Laser therapy isn’t “close enough.”
Laser therapy is exact or nothing.
And this is where offshore manufacturing often collapses under scrutiny.
Risks of Non-Compliant or Counterfeit Devices
The FDA has repeatedly warned that imported, non-compliant laser devices (including devices marketed for hair growth) may:
- exceed safe emission limits
- deviate significantly from labeled wavelength
- have poor optical uniformity
- lack critical safety interlocks
- skip the laser product reporting process
- counterfeit or imitate established devices
In fact, the global counterfeit medical device problem is so severe that both the FDA and World Health Organization (WHO) classify it as a threat to consumer safety.
Why does this matter for LPT specifically?
Because an LPT device isn’t a massager or a heat pad.
It is a precision photonic instrument calibrated to deliver a therapeutic dose window that is incredibly tight.
Half the intended irradiance?
→ Ineffective therapy.
Double the intended irradiance?
→ Possible oversaturation, nullified benefit, or tissue stress.
Random wavelength drift?
→ Light stops interacting with cytochrome c oxidase efficiently.
No traceability?
→ Consumers have no recourse if something goes wrong.
Counterfeit optics?
→ Follicles get uneven exposure, which can hinder regrowth over months of diligent use.
Perhaps the most overlooked risk is psychological:
When someone buys a low-standard or counterfeit device, uses it faithfully for weeks or months, and sees little to no improvement, they internalize a gut-level belief:
“Laser therapy doesn’t work.”
But the truth is:
The device didn’t work — not the science.
This is why U.S. manufacturing, with auditable controls and strict regulatory demands, anchors the credibility of the entire LPT category.
USA Made vs China Made LPT Devices: The Uncomfortable but Necessary Truth
If there is one moment in this entire article that deserves your full attention, it’s this one… because choosing an LPT device is not choosing a phone case or an air fryer.
It is choosing a laser-powered medical product that sits just inches from your brain, optic nerves, and a hair follicle microenvironment that responds to light with biochemical exactness.
So yes, the origin of that device matters. More than consumers have been told. More than marketing typically reveals.
And in this space (the space where precision engineering meets human biology), the contrast between U.S. manufacturing ecosystems and China-based high-volume manufacturing ecosystems becomes impossible to ignore.
Regulatory Oversight — FDA vs. NMPA/CFDA
The United States runs one of the world’s strictest medical-device oversight systems. Every manufacturer must comply with:
- FDA’s QSR (21 CFR Part 820)
- FDA’s new QMSR (effective 2026), aligning with ISO 13485:2016
- Laser safety reporting requirements
- Design controls, risk management, supplier traceability, complaint handling, and CAPA systems
This creates what is essentially a closed-loop regulatory ecosystem, where:
- every supplier must be documented
- every optical component must be traceable
- every manufacturing step is auditable
- every device is accountable
- every deviation must be corrected
In China, oversight runs through the National Medical Products Administration (NMPA), formerly CFDA. While it has strengthened dramatically over the past decade, it operates in a different enforcement culture:
- regional inconsistency
- less intrusive inspection frequency
- more industrial scalability pressures
- supply-chain opacity
- fewer design-history requirements
- less centralized post-market surveillance
This is not about criticizing a country. It is about recognizing structural differences in regulation.
The FDA’s system is intentionally rigid.
NMPA’s system is intentionally flexible.
And LPT is a therapy where rigidity outperforms flexibility every single time.
Component Quality, Supply Chains, and Traceability
China is the world leader in high-volume component manufacturing, but the same infrastructure that enables affordability also enables:
- part variability across batches
- supplier substitutions without notice
- non-uniform optical quality
- laser diode inconsistency
- lack of long-term calibration stability
And in a device that relies on a specific wavelength, exact irradiance, and consistent beam geometry, even small variances ripple into biological consequences.
What does “variability” look like in practice?
- A diode meant to emit 680 nm instead emits 665 nm.
- Irradiance advertised at 5 mW/cm² measures 2.4 mW/cm².
- Beam divergence widens over time due to cheap optics.
- Heat dissipation shifts output power after several months.
Small differences?
To a consumer, yes.
To a hair follicle trying to respond to photobiomodulation?
They might as well be different therapies.
By contrast, U.S. manufacturing under QSR/QMSR requires:
- validated suppliers
- component certification
- device history records
- standardized calibration procedures
- corrective action pathways
- traceability from diode source to final assembly
This is the only environment where a therapeutic laser dose can be guaranteed over years of use.
Safety Compliance & Laser Classification
Laser Phototherapy devices are regulated as radiation-emitting medical devices, and in the U.S., they must comply with:
- IEC 60825-1
- FDA Laser Notice No. 56
- Laser product reporting requirements
Consumers rarely see these reports but they dictate:
- maximum permissible exposure
- wavelength accuracy
- accessible emission limits
- labeling requirements
- engineering safety controls
In China-based mass manufacturing:
- IEC specs may be stated, but not verified
- third-party audits aren’t mandatory
- emission level testing can vary by facility
- design controls may be simplified for speed
It only takes one misalignment… one diode drifting off-spec… one supply batch changed without documentation…
for an LPT device to behave unpredictably.
And with LPT’s incredibly narrow therapeutic window, “almost compliant” is operationally equivalent to non-functional.
The Hidden Risk of Counterfeit & Look-Alike Devices
The majority of counterfeit laser medical devices originate in China-based manufacturing corridors.
The WHO, FDA, and OECD all acknowledge counterfeit medical devices as a major global safety issue.
Some of these imitation devices:
- copy the exterior design of legitimate helmets
- use bargain-bin diodes
- have no calibration
- lack safety interlocks
- contain unlabeled optical components
- never undergo regulatory testing
- bypass NMPA review entirely by being sold directly to U.S. consumers
This is not a criticism of China as a nation; it is a documented fact about global counterfeiting supply chains.
And consumers cannot visually tell the difference.
Not from photos.
Not from packaging.
Not from Amazon listings.
Not from AliExpress stores.
A counterfeit LPT device may look legitimate… yet emit light that delivers zero therapeutic value or, worse, emits excessive exposure outside allowable parameters.
When a therapy is dose-sensitive (as LPT is), counterfeits don’t just waste money.
They contaminate trust.
Why U.S.-Made LPT Devices Typically Outperform Offshore Devices
When the dust settles, the differences resolve into five core pillars:
1. Stricter, routinely enforced FDA oversight
No other country subjects low-level laser devices to the same depth of design controls and post-market accountability.
2. Consistent optical engineering and calibration
Manufacturers must demonstrate stable wavelength, irradiance, and beam parameters across every production batch.
3. Full traceability and documented supply chains
Every component (from diode to lens to housing) must have a traceable chain of custody.
4. Lower counterfeit exposure
U.S.-based production drastically reduces the chance that a device resembles a “generic shell” repurposed by offshore factories.
5. Legal accountability
If something fails, U.S. companies are bound by FTC, FDA, and consumer protection laws. Overseas sellers often are not.
In a therapy where light is a drug, and the scalp is sacred biological territory, you want the device delivering that light to be born in an ecosystem that can prove (not promise) its safety and consistency.
For LPT, that is the United States.
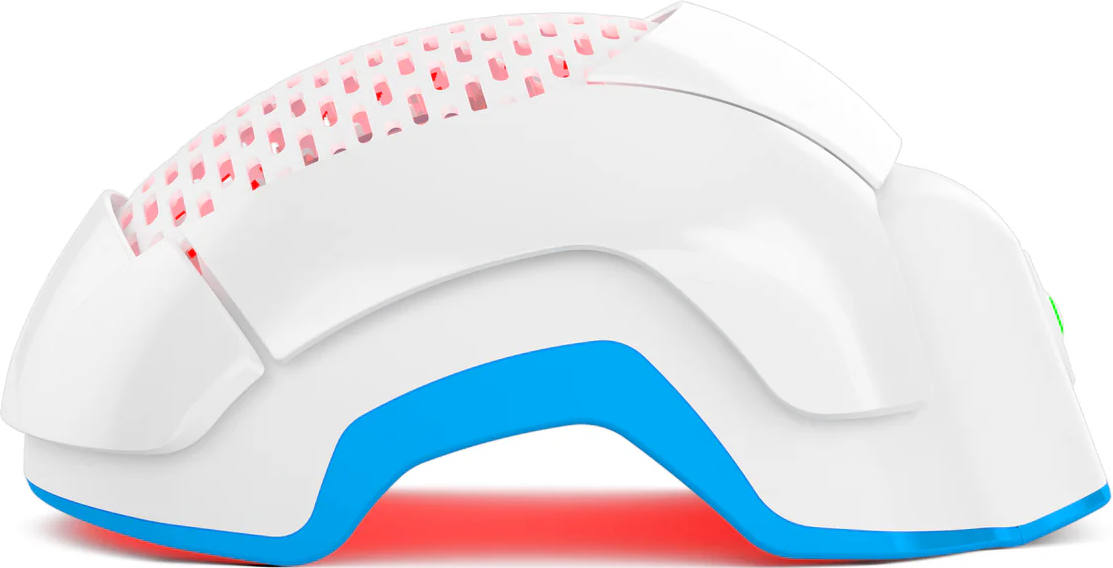
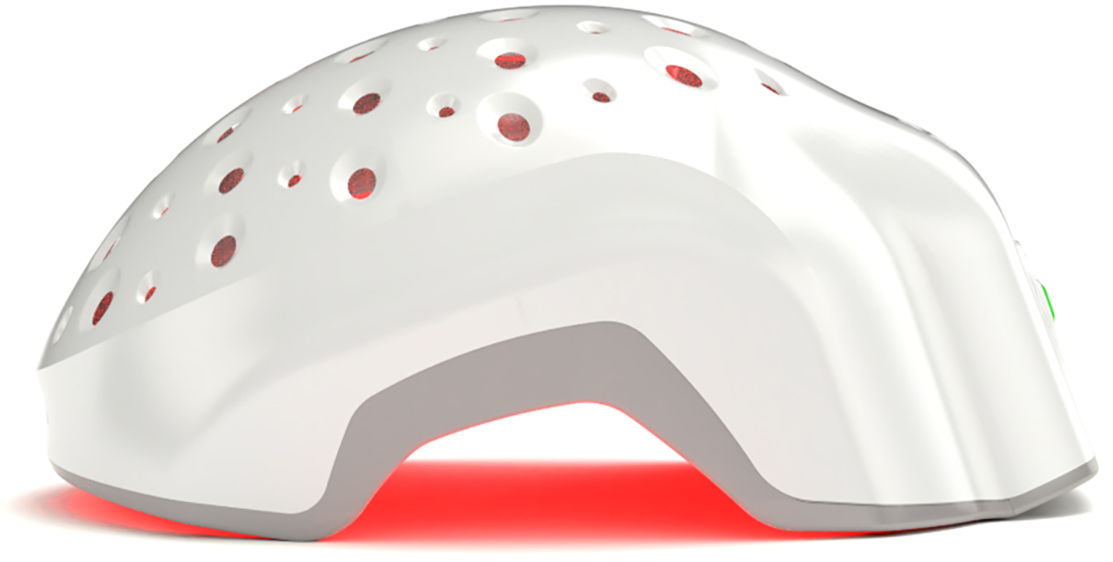
The Theradome Difference: U.S.-Made, FDA-Cleared, Engineered for Precision
Every category has its pioneer — the company that builds the technology before the industry understands why the details matter.
For wearable Laser Phototherapy devices, that company is Theradome.
And while this piece is not meant to be sales copy, it would be intellectually dishonest to discuss the technical, biological, and regulatory stakes of U.S.-based manufacturing without acknowledging the device that set the global precedent.
Theradome wasn’t just “another device.”
It was the first-ever FDA-cleared wearable LPT helmet in the world, created in Silicon Valley and engineered from the outset to meet U.S. medical device standards… even before many consumers understood why that would matter.
A few essential points stand out:
1. Designed and Assembled in the USA
Theradome isn’t simply assembled in America; its engineering, optical architecture, firmware logic, and manufacturing processes are rooted in Silicon Valley under U.S. medical-device quality frameworks. This brings something rare in the LPT category: full-spectrum domestic oversight, from concept to calibration.
Theradome is the only Laser Phototherapy device manufactured in the United States, built under the strictest safety and quality controls required by FDA-regulated systems. That ecosystem ensures that every diode, every optical path, and every calibration step meets medical-grade expectations rather than mass-production shortcuts.
The company also develops and grows its own proprietary therapeutic lasers in Silicon Valley, giving it direct control over wavelength consistency, optical purity, and long-term output stability. In practice, that means users can trust the device’s components and laser profile to deliver the FDA-cleared therapeutic parameters safely, predictably, and effectively — not just on day one, but session after session.
Exactly what LPT needs.
2. Built Under FDA-Cleared Quality Systems
The device achieved FDA clearance under stringent design controls, and its manufacturing processes align with QSR/QMSR principles, including:
- documented risk management
- calibration verification
- supplier validation
- device history records
- continuous quality audits
These are the controls that keep wavelength, irradiance, and coverage patterns consistent for years, not months.
3. Stability of Light Output
One of Theradome’s quiet strengths is its commitment to optical uniformity:
- no extreme hotspots
- no cold zones
- no diode drift that weakens dose
- no “good batch / bad batch” inconsistencies
Because the device is built in an environment that enforces manufacturing repeatability, users receive something LPT rarely offers at scale:
Predictable bioenergetic stimulation, every session.
4. Coverage & Ergonomics Based on Real Scalp Biology
Theradome’s coverage map is anatomical.
It targets the vertex, mid-scalp, and hairline regions implicated in androgenetic alopecia, distributing light in consistent patterns.
5. Transparent Accountability
If something goes wrong (a diode fails, a part degrades, a calibration shifts), the user is protected by:
- U.S. warranty systems
- U.S. consumer protection laws
- U.S. device servicing infrastructure
Offshore sellers rarely offer anything comparable.
Consumer Confidence & Trust
When you buy a device made in the United States, you aren’t only purchasing hardware.
You are purchasing:
- transparency
- predictability
- audited manufacturing
- regulated optical performance
- traceable components
- legal accountability
These are the backbone of medical-grade reliability.
In the U.S., if a device is misrepresented, emits unsafe radiation, or fails to meet its listed parameters, the manufacturer can be held accountable by:
- the FDA,
- the FTC,
- the U.S. legal system, and
- the customers themselves.
Compare that to an offshore seller shipping directly to consumers.
If it fails? If it burns out? If it does nothing?
Your recourse is often… nothing.
And in a therapy that relies on thousands of photons precisely interacting with the mitochondria of each follicle, trust isn’t a luxury.
It is a prerequisite.
Consumers don’t just buy an LPT device;
they buy the ecosystem that built it.
How to Verify Device Claims Yourself
If you want to separate real medical devices from marketing masquerades, here is the exact process experts use.
These steps require no special training… just curiosity and a willingness to look beyond polished packaging.
1. Check the FTC’s “Made in USA” Requirements
Go to the manufacturer’s website and look closely at their origin language.
Red flags include:
- “Designed in the USA”
- “Assembled in the USA”
- “Engineered in America”
These phrases do not mean “Made in the USA.”
A legitimate “Made in the USA” claim must satisfy “all or virtually all” domestic manufacturing, a demanding standard.
2. Look Up the Device in the FDA 510(k) Database
Every FDA-cleared LPT device has a 510(k) number.
Search it here:
https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm
If nothing appears, that device is not FDA-cleared regardless of what the marketing implies.
You should see:
- a predicate device
- the exact product code
- manufacturer name
- decision date
If the listing doesn’t match the product sold… walk away.
3. Confirm Laser Class & Safety Compliance
All legitimate LPT devices must reference:
- IEC 60825-1
- FDA Laser Notice No. 56
- Class 3R safety classification (for most hair-regrowth lasers)
If a device offers no information on laser class, photonic output, or emission limits, it is not a serious medical product.
4. Ask for Third-Party QC, Calibration, or Bench Testing
Reputable U.S. manufacturers often:
- perform multi-point diode calibration
- test beam uniformity
- document irradiance stability
- validate optical design
If a company cannot produce any documentation, that usually means they have none.
5. Beware Ultra-Low Prices and Mass-Market Listings
A medical-grade LPT device requires:
- calibrated diodes
- high-tolerance optics
- standardized assembly
- quality testing at multiple stages
These things are not cheap.
If a laser helmet sells for the price of a household gadget, it is almost certainly not built under medical device standards.
Conclusion
When people talk about “Made in the USA,” they often imagine patriotism, craftsmanship, maybe higher costs.
But for medical devices worn on the head (devices that emit therapeutic light across the scalp, near the eyes, near the brain), origin is a safety framework, an engineering discipline, and a biological safeguard.
And that means the device delivering that laser phototherapy must be:
- consistent
- traceable
- stable
- audited
- engineered under strict controls
In a world full of noise, shortcuts, and look-alikes, a device built with precision, audited by federal oversight, and manufactured under a culture of accountability is more than a choice.
It is the difference between light as a gimmick… and light as real medical therapy.