Some mornings, you catch yourself in the mirror and pause—wait… is my ponytail thinner than it was last month? It’s a small shock that turns into a quiet worry. If you’re on birth control pills, that creeping question follows: Can birth control cause hair loss?
The answer is complicated. Most women never notice any shedding linked to the pill. Others, especially if they have a genetic tendency toward thinning, do. And sometimes, oddly enough, the hair loss shows up after stopping birth control, not while taking it.
Here, we’re going to untangle that hormonal puzzle. By the end, you’ll understand why it happens, who’s most at risk, and what you can do to prevent it… or reverse it.
Understanding Birth Control Pills and How They Affect Hormones
Birth control pills may seem simple (just tiny tablets), but they’re really a sophisticated hormonal system in disguise. Most come in two major types:
-
Combination pills with both estrogen (usually ethinylestradiol) and a synthetic progestin.
-
Progestin-only pills, sometimes called “mini‑pills.”
Here’s where things get interesting. Estrogen in combination pills raises SHBG (sex hormone‑binding globulin), which latches onto free testosterone. Less free testosterone generally means less risk of androgenic activity in hair follicles—good news for most women.
But not all progestins are alike. Some, like levonorgestrel or norgestrel, have higher androgenic activity. In genetically sensitive women, that androgen-like effect can nudge hair follicles toward a resting phase, known as telogen. Think of it as hair hitting the “pause” button.
Meanwhile, newer progestins like drospirenone or cyproterone acetate actually have anti‑androgen properties. They’re the ones sometimes prescribed to help with acne or even mild hair issues.
The body’s response is highly individual. Two friends can take the same pill, and one will notice lush hair while the other worries about her part widening. Hormones interact with genetics, stress, diet, and subtle health factors like thyroid function.
In short, the pill changes hormone signaling in a way that can either protect your hair or, in the wrong context, trigger temporary shedding. Understanding which progestin you’re on is step one. And if you’re already thinking, “So is my hair safe?”—we’re getting there.
Can Birth Control Really Cause Hair Loss? The Science Behind It
Hair growth isn’t just cosmetic—it’s biological theater. Each strand cycles through three phases:
Anagen (growth), Catagen (transition), and Telogen (resting/shedding).
Most hair sits in the growth stage, happily sprouting for years. But when hormones shift—like when starting a new birth control pill—more hairs can slip prematurely into telogen. This is telogen effluvium (TE), and it shows up as diffuse shedding a few months later.
Clinical evidence backs this up. A classic JAMA study from 1967 first flagged oral contraceptives as a possible trigger for female hair loss. Modern dermatology still recognizes TE as a potential, though relatively rare, side effect—especially in those with androgen sensitivity or family history of female pattern hair loss.
There’s another layer. Certain progestins with higher androgenic properties can accelerate underlying androgenetic alopecia (the female version of pattern hair loss). That doesn’t mean birth control creates the condition—but it can unmask it sooner.
And stopping the pill can also cause shedding. When hormone support suddenly drops, follicles that had been “coasting” on stable estrogen levels reset their cycle all at once. Cue another round of TE.
So yes—birth control pills can cause hair loss, either by triggering TE or amplifying genetic thinning. But it’s not universal. Most shedding is temporary, and knowing your pill type—and your risk profile—makes all the difference.
Can Stopping Birth Control Cause Hair Loss Too?
It feels almost unfair, doesn’t it? You finally decide to come off birth control, expecting your body to thank you with a return to “normal,” and instead, you start noticing more strands in the shower drain.
Here’s why that happens.
When you stop taking birth control, your body experiences a sharp hormonal shift—estrogen levels dip, and the stable hormone environment the pill provided disappears almost overnight. Hair follicles that had been quietly coasting along in the growth (anagen) phase can abruptly slip into telogen (resting). This sudden, synchronized shift is called post‑pill telogen effluvium. It usually shows up 2–3 months after stopping and peaks around the 3‑ to 6‑month mark.
Good news is… in most cases, this shedding is temporary. As your body recalibrates, new hairs enter the growth phase again. Clinical observations show that for most women, the shedding stabilizes within six to nine months—though it can feel like forever while it’s happening.
Some women never notice a thing. Others experience a full “hair freak‑out,” especially if they have an underlying genetic tendency toward androgenetic alopecia. In those cases, the post‑pill fallout may feel more severe or last longer.
So yes, stopping birth control can trigger hair loss—but it’s usually your body adjusting, not permanent damage. The key is knowing how to spot it, and when to act.
Who Is Most at Risk for Birth Control‑Related Hair Loss?
Not every woman on birth control will face hair loss. In fact, the majority glide through without a single stray worry. But some people are more vulnerable.
Genetic predisposition is the biggest factor. If women in your family—mother, grandmother, sisters—have experienced female pattern hair loss or thinning with age, your follicles may be more sensitive to even subtle androgen changes.
Other risk enhancers include:
-
PCOS or hormone imbalances, where androgens are naturally higher.
-
Thyroid issues or anemia, which already stress the hair cycle.
-
Severe stress or crash dieting, which can compound telogen effluvium.
And high‑androgenic progestins (like levonorgestrel or norgestrel) are more likely to amplify shedding in genetically sensitive women. By contrast, low‑androgenic or anti‑androgenic pills (drospirenone, cyproterone acetate) are less likely culprits and sometimes even protective.
So if your hairline has always been rock‑solid and your family history is clear, your risk is lower. But if you’re already predisposed (or juggling other hair stressors) birth control can act as the final trigger that makes shedding noticeable.
How to Tell If Your Hair Loss Is from Birth Control or Something Else
Hair loss can feel like an unsolvable mystery. But timing and pattern usually give you clues.
Telogen effluvium (the most common pill‑related shedding) presents as diffuse hair loss all over the scalp, not isolated patches. You’ll notice extra hair in your brush, on your pillow, or in the shower 2–4 months after starting or stopping birth control. It’s a slow drift rather than a sudden bald spot.
Compare that to androgenetic alopecia, which usually shows thinning at the part line or crown. Birth control doesn’t cause this genetic condition, but high‑androgen pills can accelerate its appearance.
How do you confirm the source?
-
Check the timeline: Did shedding start a few months after a pill change or discontinuation?
-
Assess your health: Rule out thyroid issues, iron deficiency, or major stress events in the same timeframe.
-
Seek professional input: Dermatologists and trichologists can run a pull test, examine scalp density, and order lab work if needed.
And here’s the tricky part: hair loss is often multifactorial. Birth control may be the spark, but diet, stress, and underlying health all play supporting roles.
If you’re unsure, keep a simple hair diary noting the shedding pattern and any life changes. Patterns over weeks often tell the story clearly than a single anxious glance in the mirror.
Preventing Hair Loss from Birth Control Pills
If you’re just starting the pill (or thinking about switching) there’s a lot you can do to stack the odds in your favor. Hair loss isn’t inevitable.
Step one: Know your progestin. Not all birth control pills carry the same risk. Pills containing high‑androgenic progestins like levonorgestrel or norgestrel are more likely to spark shedding in sensitive women. By contrast, drospirenone or cyproterone acetate formulations are considered lower‑risk—or even slightly protective for those with mild androgen sensitivity. (It’s the quiet detail your doctor might not always emphasize.)
Step two: Protect your baseline health. Hair follicles thrive on balance.
- Make sure iron, vitamin D, and thyroid levels are in check.
- Avoid crash dieting—your follicles notice.
- Keep stress in check. Cortisol spikes can compound telogen effluvium.
Step three: Plan your transitions. If you intend to stop birth control, consider consulting your doctor about a gradual strategy. While there’s no foolproof way to dodge post‑pill shedding, smoother hormonal changes can sometimes reduce the shock to your follicles.
And here’s an underrated tip: pay attention to your hair early. A subtle widening of your part or a few extra hairs on your pillow isn’t always cause for panic—but noticing patterns sooner helps you make proactive changes before shedding peaks.
Truth is, prevention is often a mix of smart pill selection, lifestyle tuning, and a dash of patience. Hair loves stability.
Managing and Treating Hair Loss After Birth Control
If shedding has already set in, don’t despair. Most pill‑related hair loss is temporary, and follicles are surprisingly resilient.
Natural Recovery Timeline
Telogen effluvium usually self‑resolves within six to nine months as your hormones stabilize. It’s frustrating, yes, but think of it as your scalp re‑syncing its calendar. New hair will push through as older strands finish shedding. Patience is part of the treatment plan.
Medical Treatments
Persistent shedding—or visible thinning along the part—can benefit from intervention. Topical minoxidil (2% or 5%) is one of the most studied options for stimulating regrowth, and it’s often recommended even in temporary TE if the shedding feels extreme. For women with signs of androgen‑driven thinning, doctors may prescribe spironolactone, which reduces androgen impact at the follicle level.
A trichologist or dermatologist can confirm your diagnosis, run lab work (thyroid, ferritin, vitamin D), and monitor your progress. Self‑diagnosing often leads to unnecessary panic—or worse, unhelpful supplements.
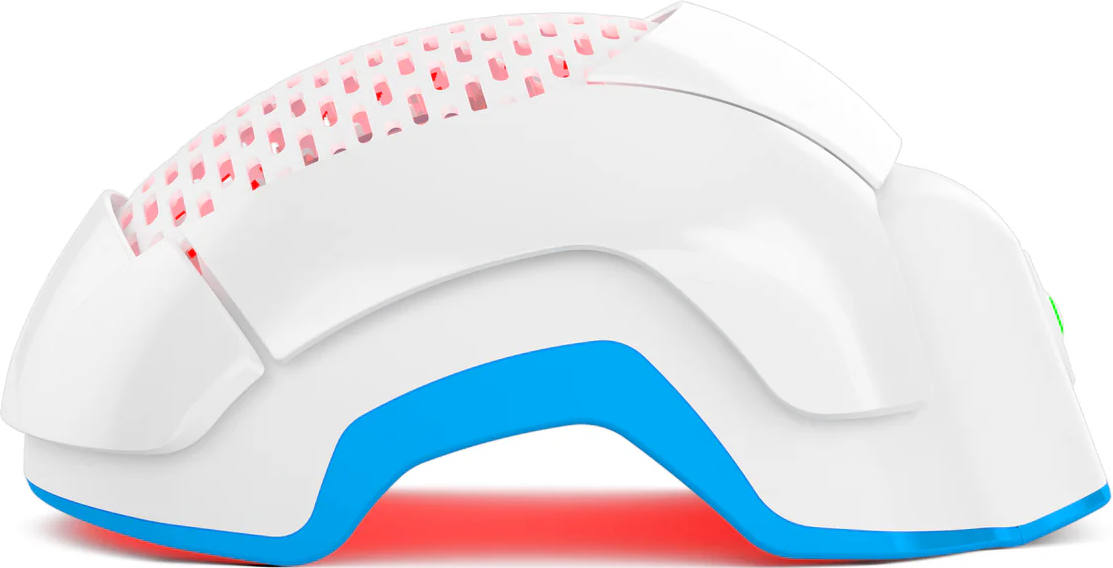
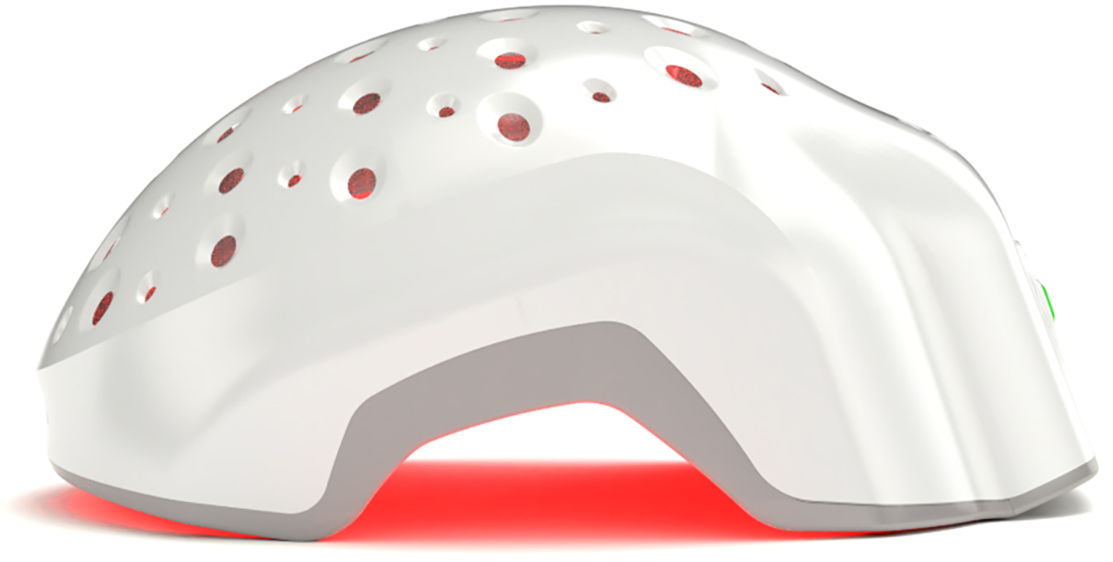
Non‑Hormonal Options like Laser Phototherapy (LPT)
Laser Phototherapy (LPT). Unlike drugs, LPT works by photobiostimulation, nudging dormant follicles back toward growth without altering hormones. FDA‑cleared wearable devices like Theradome deliver light directly to the scalp and are clinically shown to improve density over months. It’s painless, non‑invasive, and pairs well with other treatments.
Consider LPT as part of a layered recovery strategy: healthy lifestyle, medical evaluation, and consistent therapy. With time, most women see significant improvement.
Emotional and Psychological Support During Hair Shedding
Here’s the part people rarely talk about: hair loss can hit emotionally as hard as physically. That daily reminder in the shower drain feels intimate and unfair.
Acknowledge the stress—don’t bottle it. Even temporary shedding can stir anxiety, self‑consciousness, or social withdrawal. Studies have linked female hair loss to lower self‑esteem and mild depression, so it’s not “just vanity.”
Simple steps help.
- Track progress with photos to see regrowth that’s easy to miss day‑to‑day.
- Share your concerns with someone you trust—or a support group.
- Consider mindfulness or stress‑management practices, which also indirectly help your follicles.
And if it’s taking a heavy toll, talk to your doctor. Emotional health is part of treatment too. Sometimes, just understanding the science behind what’s happening is enough to lift some of that weight.
Conclusion
So—can birth control pills cause hair loss? Yes, sometimes. Usually as telogen effluvium or, rarely, by accelerating genetic thinning.
But the full story is more hopeful:
- Most cases are temporary.
- Pill choice matters. Lower‑androgen options reduce risk.
- Healthy habits and early attention help minimize shedding.
- Effective treatments exist— LPT.
So, don’t panic, don’t self‑treat blindly, and don’t make sudden pill changes without medical advice. If your hair feels like it’s turning against you, a trichologist or dermatologist can guide you through recovery.
Your hair story isn’t over—it’s just in a temporary chapter.