Short answer is… not exactly.
But if you’ve recently started spironolactone and are suddenly finding more hair in your brush, you’re probably wondering if something’s gone terribly wrong. You're not alone—and you’re not imagining it.
This article walks you through the science, what spironolactone does to hair, what it doesn’t do, and why temporary shedding might show up uninvited... only to fade with time. We’ll also explore what to expect long term, when it works best, and how treatments like Laser Phototherapy (LPT) can complement or even replace systemic options.
What Is Spironolactone—and Why Is It Used for Hair?
Originally developed as a potassium-sparing diuretic, spironolactone was intended for things like high blood pressure and heart failure. But something interesting happened along the way—dermatologists noticed its side effects included… less oil, fewer breakouts, and even reduced hair shedding in some women.
And no, this wasn’t accidental.
Spironolactone acts as an antiandrogen, meaning it blocks the activity of male hormones like DHT at the skin and scalp. DHT is a prime suspect in the case of female pattern hair loss (FPHL)—where it miniaturizes follicles over time, leading to thinning, especially around the part line.
Here’s where it gets interesting: spironolactone is not FDA-approved for hair loss, but it is widely prescribed “off-label” because mounting clinical evidence supports its effectiveness—especially in women with signs of androgen excess (PCOS, adult acne, hirsutism).
It’s like a DHT bodyguard, standing between your hair follicles and the hormonal chaos that wants to shrink them out of existence.
Important to note: It’s not a universal cure-all. But in the right candidate, spironolactone can help stabilize shedding, thicken strands, and (with patience) turn the tide.
The Core Question: Can Spironolactone Cause Hair Loss?
Let’s get this out of the way: there’s no solid evidence that spironolactone causes permanent hair loss. Quite the opposite—it’s routinely prescribed to treat it.
So why do some people swear their shedding worsened after starting?
Ah. That’s the rub.
What you're likely experiencing isn't true loss—it’s transient shedding, a temporary uptick in hairs exiting the scalp that’s actually tied to hair cycle synchronization.
Here’s how that works: when a treatment like spironolactone begins correcting hormonal imbalances, it can kick some follicles out of telogen (resting) and into anagen (growth). But to get there, the old hair has to fall first. This process, known as telogen effluvium, feels scary—but it’s typically short-lived and self-limiting.
In clinical studies, particularly ones combining spironolactone with low-dose oral minoxidil, early shedding showed up in the first 4–8 weeks and settled soon after (Sinclair et al., 2018). Importantly, this didn’t predict treatment failure. In fact, it often preceded visible improvements later.
That said—if shedding persists beyond 12–16 weeks or worsens dramatically, a professional evaluation is warranted. Occasionally, other culprits like iron deficiency, thyroid dysfunction, or stress-related telogen effluvium are also at play.
So no—spironolactone doesn’t cause hair loss in the damaging sense. But it might shake things up a little before the real growth begins.
Does Spironolactone Actually Help With Hair Growth?
In a word? Yes.
But let’s unpack that, because “growth” can mean different things depending on who’s asking.
Clinical research consistently supports spironolactone’s ability to help stabilize female pattern hair loss (FPHL) and, in many cases, promote visible thickening. In one systematic review (Aleissa et al., 2023), 42% of patients reported mild improvement and 31% saw increased hair density.
That’s not insignificant.
Typical doses range from 50 to 100 mg/day, though dermatologists often start low and titrate slowly. The goal is to minimize side effects while gradually improving hair density over a 6–12 month window.
Important detail: success with spironolactone doesn’t mean dramatic regrowth overnight. It usually looks like fewer hairs on your pillow, a thicker part line, and a general sense that things have… calmed down.
You may not notice it day to day. But over months, the before-and-after photos often tell a different story.
Interestingly, spironolactone seems to be especially helpful in women with signs of androgen sensitivity—things like acne, oily skin, irregular periods, or hirsutism. This makes sense, given that the drug's mechanism targets androgen receptors and 5-alpha-reductase activity—two players involved in miniaturization.
Also worth noting: spironolactone plays well with others. When used alongside topical minoxidil, low-dose oral minoxidil, or Laser Phototherapy (LPT), response rates improve.
If you’re dealing with chronic, progressive thinning and are a good candidate—spironolactone is a legitimate, evidence-based option. Just don’t expect miracles in month two.
What Kind of Hair Loss Does Spironolactone Treat?
Spironolactone is not a one-size-fits-all fix. It’s specifically useful for androgen-driven thinning—aka female pattern hair loss (FPHL).
FPHL typically shows up as:
- Widening of the part
- Diffuse thinning on the crown
- Miniaturized hairs that never quite grow to full length
Unlike patchy bald spots (like alopecia areata) or massive shedding (like post-viral telogen effluvium), FPHL is slow and sneaky. Which is exactly why many people don’t catch it until they’ve already lost 20–30% of their density.
Now, here’s the catch:
Spironolactone won’t help if your shedding is caused by other things—like stress, crash dieting, thyroid issues, iron deficiency, or autoimmune disease. In fact, starting it without a proper diagnosis can delay the treatment you actually need.
That’s why most trichologists recommend getting a formal evaluation before starting any antiandrogen. Bloodwork, history, scalp exam—yes, it's worth it.
Who Should Consider Spironolactone for Hair Loss?
Okay, so who actually makes a good candidate?
If you’re a woman under 45 dealing with chronic thinning, maybe with signs of hormonal imbalance (irregular periods, adult acne, excess facial/body hair), you might be a great fit.
Spironolactone is also widely used in women with PCOS—partly for metabolic support, but often to address unwanted hair loss and hirsutism.
On the other hand… not everyone is an ideal match.
Men? Not so much. The risk of gynecomastia, reduced libido, and other feminizing side effects usually outweighs the benefits—so dermatologists typically prefer finasteride or dutasteride in male AGA cases.
Postmenopausal women can sometimes benefit from spironolactone, too—but it requires closer monitoring, especially around blood pressure and potassium levels. And anyone with renal disease, low blood pressure, or certain medications (ACE inhibitors, potassium-sparing diuretics, etc.) needs careful consideration.
It’s not over-the-counter shampoo. It’s a prescription drug with real effects—good and bad.
So talk to a trichologist or dermatologist, who knows hair, hormones, and the nuances in between.
What About Side Effects, Interactions, and Monitoring?
This is where spironolactone goes from “interesting” to “requires respect.”
Let’s break it down.
Common side effects:
- Fatigue, especially when starting or increasing your dose
- Breast tenderness
- Dizziness (because it lowers blood pressure)
- Irregular periods, which often stabilize over time or with the addition of a hormonal contraceptive
- Increased urination (it’s a diuretic, after all)
These are manageable for most. But don’t power through blindly—tell your provider if something feels off.
What about potassium?
Ah, the infamous hyperkalemia risk. Here’s the nuance most blogs skip:
In healthy women under 45 without kidney disease or potassium-raising meds (like ACE inhibitors), the risk is… surprisingly low. One landmark study in dermatology (Plovanich et al., 2015) found that potassium levels rarely budged in this group—even with long-term use.
So, in many cases, routine potassium monitoring may not be necessary after a normal baseline. However—(and this is a big however)—things change if you’re older, taking interacting meds, or dealing with renal concerns.
In those cases, potassium checks become essential.
So who needs more frequent labs?
- Age 45+
- On ACE inhibitors, ARBs, or drospirenone-containing birth control pills
- Have kidney or adrenal disorders
- On high-dose spironolactone (>100 mg/day)
It’s not about fear—it’s about tailoring safety to your body and lifestyle.
Pregnancy?
Avoid completely. Spironolactone can potentially feminize a male fetus in utero. If you’re of childbearing potential, use reliable contraception—period. No guessing.
Breastfeeding?
Actually… yes, in most cases. The LactMed database and cardiology guidelines say spironolactone and its metabolite canrenone pass into breast milk in extremely low amounts and aren’t likely to cause harm. But again, individualized advice is key.
Side effects and interactions aren’t meant to scare you—they’re just a reminder: this isn’t a supplement. It’s a prescription drug with a solid track record... and a few footnotes worth reading closely.
Dosing, Duration, and What to Expect
Start low.
Most hair specialists begin patients on 25 mg once daily, then increase to 50 or even 100 mg/day based on tolerance and results.
If your doctor starts you at a higher dose right away... maybe ask why.
Because while higher doses may act faster, they also raise the risk of side effects—and slow and steady usually wins the scalp.
How long before I see results?
This part can feel like watching water boil.
You’ll likely need 6 to 12 months to see meaningful changes—reduction in shedding, improvement in density, or visible thickening at the part line. Sometimes it happens sooner. But… more often, it’s a game of patience.
(And yes, early shedding may still show up around weeks 4–8)
Pro tip: take photos in the same lighting every 4–6 weeks. That’s how you spot progress you didn’t realize was happening.
Oh—and if you stop?
Spironolactone isn’t a permanent fix. If you discontinue it abruptly, shedding may return, sometimes with a vengeance. Some providers recommend tapering slowly; others simply monitor for signs of recurrence and restart if needed.
Don’t panic if you miss a day here and there. But don’t quit cold turkey without a plan either.
Can You Combine Spironolactone With Other Hair Treatments?
Absolutely—and in many cases, that’s the best approach.
Hair loss is rarely one-dimensional. So if you want to attack it from multiple angles? Spironolactone can play well with others.
Most common pairings:
- Topical minoxidil (Rogaine): stimulates follicles directly
- Low-dose oral minoxidil: emerging therapy, often paired with spironolactone in studies
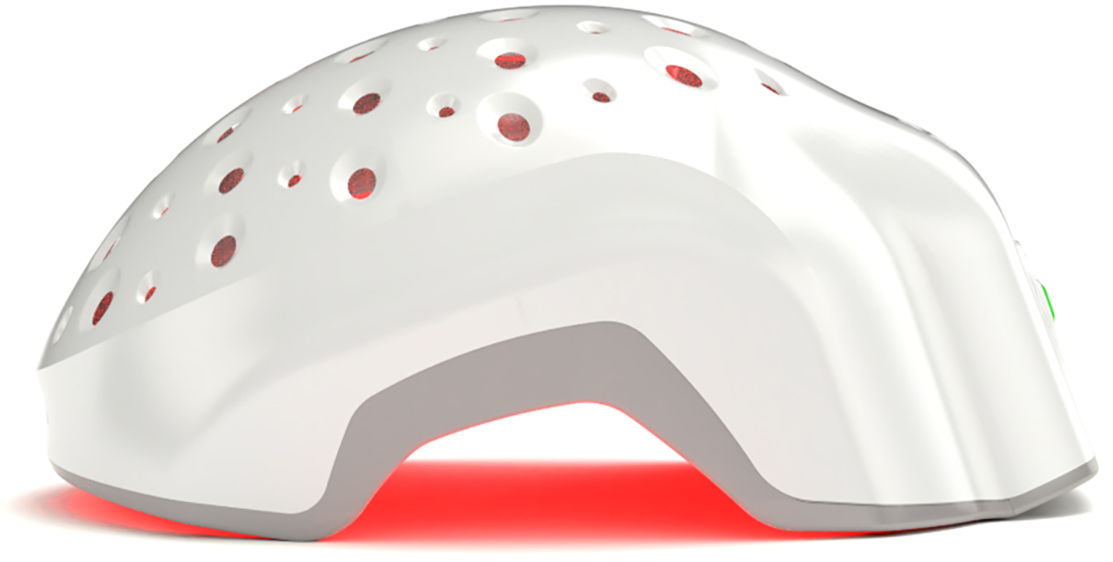
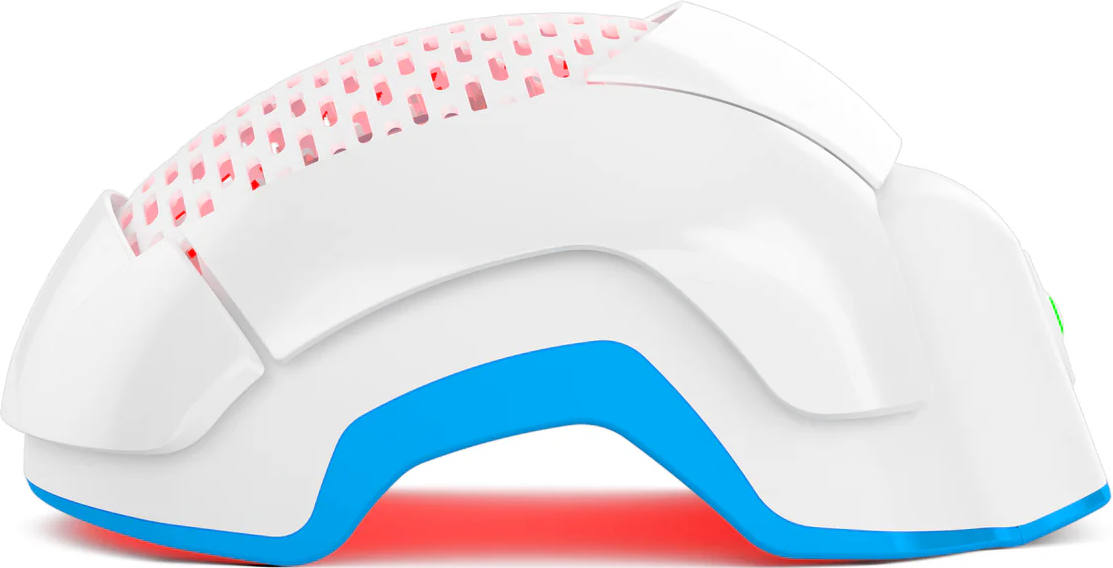
- Laser Phototherapy (LPT): promotes regrowth through red light-based stimulation
- Microneedling: boosts delivery of topicals and triggers healing cascades
In fact, in a study by Sinclair et al. (2018), women taking low-dose oral minoxidil plus spironolactone saw improvement in both shedding and Sinclair grade—despite some early hair fall in the beginning. The combo outperformed monotherapy in several reviews.
Laser Phototherapy adds another dimension here. It’s drug-free, painless, and works by enhancing cellular energy production. It’s like strength training for your scalp cells—especially effective when paired with medications like spironolactone.
So no, it’s not “either-or.”
You can absolutely layer treatments... intelligently.
But do it with a strategy. One that considers mechanisms, tolerance, and your personal health profile—not just what influencers swear by.
What If Spironolactone Isn’t Right for You?
Not every treatment fits every head.
And while spironolactone helps a lot of people, it's not the end of the line if it’s not for you. Whether it's contraindicated (pregnancy, kidney issues, or conflicting meds), not tolerated, or simply doesn’t work—you've got options.
Viable alternatives include:
- Topical minoxidil: Still one of the most researched options for both men and women. Available OTC. It’s messy, yes—but effective.
- Low-dose oral minoxidil: Gaining popularity for women who can't tolerate the topical version. Often prescribed off-label by trichologists and dermatologists.
- Laser Phototherapy (LPT): For those who want to avoid drugs entirely or stack their regimen, LPT is a no-pill, no-hassle tool that actually stimulates follicular regrowth.
- PRP (Platelet-Rich Plasma) and microneedling: These are more invasive—and can get pricey—but some patients swear by the results. Clinical data is mixed, but not dismissible.
Also, let's not forget the low-hanging fruit—those lifestyle or nutritional factors that sabotage progress when left unchecked.
Low iron? Especially ferritin under 40 ng/mL? That can stall everything. Thyroid irregularities? Same deal. And stress? Don’t even get us started…
Yes, spironolactone is a great tool—but not the only one. A skilled provider should help you build a strategy based on your biology, not just your hairbrush.
Conclusion
Hair loss messes with more than just your appearance. It chips away at confidence, comfort, and control.
So it makes sense that shedding after starting a new treatment like spironolactone would feel... terrifying.
But here’s the thing: that early shed is not failure. It’s biology doing a bit of housecleaning.
Spironolactone doesn’t cause permanent hair loss. It treats it. And when combined with proven tools like Laser Phototherapy (LPT)—you give your follicles multiple ways to bounce back.
We won’t promise miracles.
But we will say this: if your hair is thinning, and your hormones are playing games, there are ways to get ahead of it. Spironolactone might be one of them.
Just… give it time. Track your progress. Don’t panic if week six feels worse than week one.
Real change takes months. But so does most worthwhile transformation.
And no—you’re not crazy for caring this much. That part? That’s human.