Most people still think hair loss in women is rare. It’s not. It’s just rarely talked about without a cringe or a cliche. And no—it's not always stress, age, or “maybe try more collagen.” The truth is, there are several types of hair loss in women, and lumping them all together is how people end up stuck, shedding, and Googling fixes that don’t work.
The causes vary—hormones, immune glitches, chronic tension, nutrient gaps, or just pure bad genetic luck—but what doesn’t vary is how overlooked this issue is in women. Hair loss isn’t just a cosmetic concern. It messes with your confidence, your mental health, and your sense of control.
So, this article breaks down the five most common types of hair loss in women—what causes them, how to spot them, and most importantly, what you can actually do about it.
Understanding Hair Loss in Women
Hair loss in women doesn’t always come with a receding hairline or bald crown. It’s stealthier than that. A widening part, more scalp showing, a thinner ponytail—these are clinical symptoms that often go ignored. And before you chalk it up to aging, you should know this: there are several medically recognized types of hair loss in women, and not all of them are age-related or permanent.
Unlike male hair loss, which tends to follow predictable patterns, female hair loss tends to be more diffuse and emotionally loaded. Women are hit with hormonal swings, autoimmune flares, postpartum crashes, and yes—social shame. All while being told, “It’s probably just stress.”
Look, it’s not always stress. And even when it is, that doesn’t make it less real or less treatable.
Here are the top five culprits.
1. Androgenetic Alopecia (Female Pattern Hair Loss)
This is the most common—and the most chronically misunderstood—form of hair thinning in women. Also called female pattern hair loss, it usually kicks in around menopause but can start earlier, especially if you’ve inherited it from either parent (yes, both sides count).
What makes it different from male pattern baldness? Women don’t go full cue-ball. Instead, the hair gradually thins at the crown and temples, the part line widens, and the density drops without dramatic bald patches. It’s a slow fade, not a sudden exit.
The root cause is sensitivity to androgens (male hormones that women naturally produce too). These hormones miniaturize hair follicles, shortening the growth phase and weakening hair over time. It’s hormonal, genetic, and progressive.
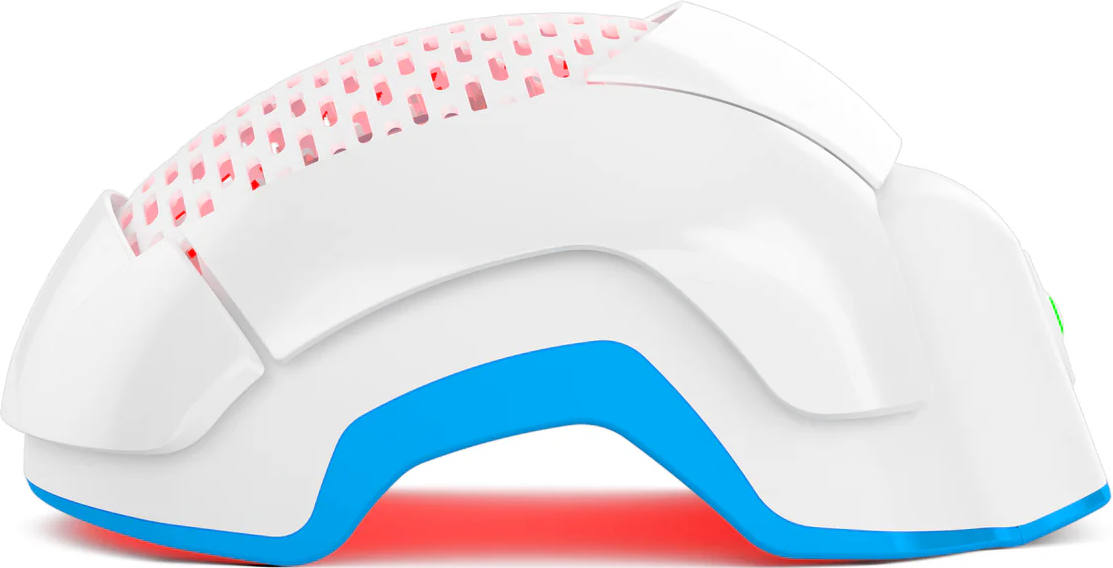
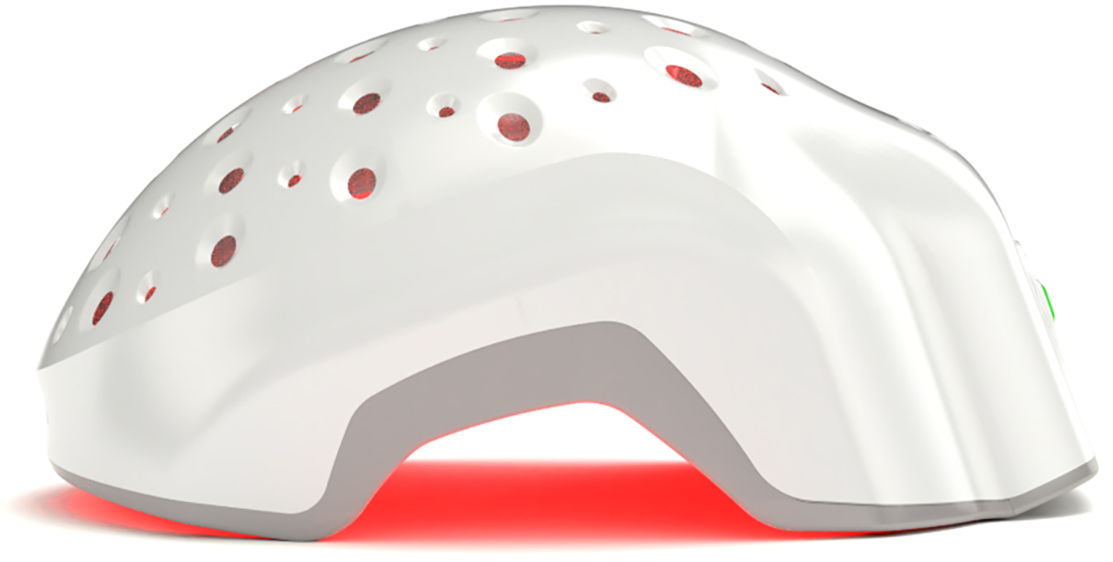
Treatments include topical minoxidil (FDA-approved for women), anti-androgens like spironolactone (under a doctor’s care), and low-level laser therapy (LLLT) or laser phototherapy (LPT), which helps stimulate miniaturized follicles back into growth.
2. Telogen Effluvium in Women
Telogen effluvium is not a disease—it’s a shock response. When your body goes through something intense (fever, surgery, illness, crash dieting, trauma), it throws a tantrum at the follicular level. More follicles than usual are pushed into the telogen (resting) phase, which leads to diffuse hair shedding about 2–3 months after the trigger.
You’ll notice more hair on your pillow, in the drain, or on your brush—but no obvious bald spots. The good news is… telogen effluvium is often temporary. The bad news? If the underlying cause isn’t identified and corrected, it can become chronic.
Stress-related hair loss in women also falls under this umbrella. Emotional or psychological stress can do just as much damage as physical trauma, and yes—it’s absolutely valid.
Recovery involves restoring balance: correcting deficiencies (like iron or B12), eating properly, managing stress, and letting time do its thing. And please, stop skipping meals.
3. Alopecia Areata in Women
This one’s autoimmune—and completely unpredictable. Alopecia areata in women happens when the immune system goes rogue and attacks your hair follicles, usually resulting in round or oval bald patches. It can hit the scalp, eyebrows, or even lashes. Sometimes it’s temporary. Sometimes it escalates.
It’s not contagious. It’s not caused by poor hygiene. And it has nothing to do with shampoo choice, despite what your neighbor’s cousin swears by.
What’s cruel about alopecia areata is that it often strikes without warning and can flare repeatedly. It’s more common in people with other autoimmune conditions, but not exclusive to them.
Treatments range from topical steroids and corticosteroid injections to emerging options like JAK (Janus kinases) inhibitors. Some patients also respond well to light-based therapies—but the earlier it’s caught, the better your odds of follicle survival.
4. Anagen Effluvium & Traction Alopecia in Women
Two very different beasts, but both cause sudden hair loss.
Let’s start with anagen effluvium, which is rapid hair shedding during the growth (anagen) phase. It’s usually triggered by chemotherapy or radiation—treatments that stop fast-dividing cells in their tracks, including hair matrix cells. Anagen effluvium causes include cancer treatment, toxin exposure, or severe autoimmune disease.
Hair usually regrows after the trigger ends, but regrowth quality and timeline can vary depending on follicle damage.
Now to traction alopecia in women—a slow, entirely preventable form of hair loss caused by chronic tension on the hair. Tight braids, high ponytails, extensions, weaves, buns—over time, they cause follicular trauma. This usually starts at the hairline or temples and can become permanent if the tension doesn’t stop.
So, stop yanking your scalp. Switch to looser styles and let your follicles breathe. Early intervention is key—if caught soon enough, hair can regrow. If you continue to keep tension on your hair follicles, over time you risk scarring and permanent damage to your ability to regrow that hair follicle.
5. Hormonal & Postpartum Hair Loss
Hormones control everything—especially your hair. Fluctuations in estrogen, progesterone, and androgens can flip the follicle switch from growth to shed with almost surgical precision.
Hormonal hair loss in women is common in PCOS, menopause, thyroid dysfunction, and yes—after pregnancy.
Postpartum hair loss usually kicks in 2–4 months after delivery. During pregnancy, estrogen levels keep hair in the growth phase longer than usual. Once levels crash post-birth, the backlog of hair enters the shed phase all at once. It’s abrupt. It’s shocking. But it’s normal—and usually self-resolving within 6–12 months.
Still, if the shedding feels extreme, if you’re seeing scalp, or if it doesn’t slow down after a year—get your iron, thyroid, and hormone levels checked. Postpartum doesn’t mean powerless.
Conclusion
Hair loss in women isn’t rare. It’s just routinely dismissed, misdiagnosed, or drowned in bad advice. Whether you’re dealing with hormones, trauma, autoimmunity, or tight hairstyles—labeling the type correctly matters. These five aren’t the only causes, but they’re the most common. And each one has its own set of triggers, symptoms, and treatments.
Stop blaming yourself. Start paying attention to the pattern. Hair loss doesn’t always mean baldness—but ignoring it almost always makes it worse.
You've got options like medications and surgical treatments. But they might not be ideal for everyone. Theradome laser hair growth devices offer a non-invasive, FDA-cleared solution for stimulating hair regrowth. Thousands have already restored their hair with Theradome. If you're ready to get healthy hair regrowth, Theradome can help you with it.