Hair loss. Even just the phrase can trigger that quiet wave of worry we all pretend not to feel. And it’s no wonder—few things unsettle our sense of self as much as finding more strands in the shower drain than on our heads. In that search for answers, vitamins often take the spotlight. Vitamin D, iron, zinc… and yes, Vitamin A. But here’s the tricky bit—Vitamin A is both hero and potential villain in the hair story.
So, does Vitamin A cause hair loss, or is it actually the missing puzzle piece your follicles have been begging for? The truth isn’t as simple as a “take more” or “avoid it entirely” situation. In fact, both deficiency and excess can play very different roles in hair health.
Vitamin A is essential for cell growth, immune support, and scalp function. Your hair follicles—tiny, active factories—rely on it for keratin production and a healthy oil balance.
But (and here’s where things get a little ironic), overdoing it can flip the switch from growth to shedding. Too much Vitamin A can nudge follicles prematurely into a resting phase, leading to diffuse hair loss known as telogen effluvium.
Before you panic and toss your supplements (or sprint to the vitamin aisle), let’s break this down properly. What exactly is Vitamin A, why does it matter for hair, and when does it tip from helpful to harmful?
What is Vitamin A and Why Does it Matter for Hair?
Vitamin A isn’t one single compound—it’s a family of fat‑soluble retinoids your body needs in measured amounts. Two main forms make their way into your diet: preformed Vitamin A (retinol, retinyl esters) from animal sources like liver, eggs, and dairy; and provitamin A carotenoids (like beta‑carotene) from colorful fruits and vegetables—carrots, sweet potatoes, spinach. The body cleverly converts carotenoids to active retinol only as needed, which is why plant sources rarely trigger toxicity.
Hair follicles are metabolically active little structures. They need Vitamin A for:
-
Keratin synthesis, the protein that literally forms each strand.
-
Sebum regulation, which keeps the scalp from drying out or flaking.
-
Cellular growth and repair, ensuring the follicle lining remains functional.
Interestingly, this vitamin has a Goldilocks quality—both too little and too much can nudge your hair cycle off balance. Optimal levels help maintain the anagen phase (growth stage), while excessive intake may prematurely shift follicles into telogen (resting) mode.
The recommended daily allowance (RDA) hovers around 700 µg RAE for women and 900 µg RAE for men. “RAE” stands for retinol activity equivalents, a way of comparing animal and plant sources. For context, a small portion of beef liver can surpass an entire day’s needs—so it doesn’t take much to tip into excess if supplements or fortified foods enter the mix.
In essence, Vitamin A is a double‑edged nutrient. It’s foundational for hair health, but it comes with a clear caution label: balance matters more than brute force.
Can Vitamin A Deficiency Affect Hair?
While deficiency isn’t the poster child for hair loss in developed countries, it can quietly set the stage for brittle strands and sluggish growth. Vitamin A supports sebaceous gland activity, which maintains a hydrated, flexible scalp. Follicles may experience dryness, and hair shafts can lose their resilience—snapping or shedding more easily) due to insufficient Vitamin A
Severe deficiency, though uncommon in places with nutrient‑rich diets, can arise in certain conditions:
- Chronic malabsorption syndromes (like celiac disease or pancreatic insufficiency).
- Extremely restrictive diets or eating disorders.
-
Liver disease, which affects Vitamin A storage.
Symptoms tend to reveal themselves subtly. Dry eyes, flaky skin, night blindness—and in advanced cases—diffuse hair thinning that resembles telogen effluvium. Importantly, hair loss from deficiency is usually part of a larger clinical picture rather than the very first sign.
Research, including dermatology reviews and case studies, aligns with this: hair changes linked to deficiency often resolve when levels normalize, though the timeline can range from weeks to months, depending on the extent of follicular miniaturization and individual health status.
Still, it’s worth noting that deficiency‑related hair loss is relatively rare compared to excess‑related shedding in supplement‑savvy populations. Most readers worried about Vitamin A and hair loss are far more likely to face the consequences of too much rather than too little. But understanding the foundational role it plays in follicle health is the first step in building—or protecting—a resilient mane.
Does Too Much Vitamin A Cause Hair Loss?
It sounds almost unfair, doesn’t it? A nutrient your body genuinely needs (one that fuels skin renewal, immunity, and even vision) can turn on you if you overdo it. Yet this is exactly the paradox of Vitamin A and hair loss.
When intake creeps above safe levels, something rather subtle but destructive can happen inside your scalp. Hair follicles that were happily in anagen phase (active growth) can be nudged prematurely into telogen phase, the resting stage. Once enough follicles go into “rest mode,” diffuse shedding begins—often suddenly, and frustratingly all over the head instead of in neat patches. Dermatologists refer to this pattern as telogen effluvium, and excessive Vitamin A intake is a known trigger.
Hypervitaminosis A Explained
Hypervitaminosis A is the medical term for Vitamin A toxicity. It doesn’t take a laboratory accident or some exotic diet to get there; it can simply creep up on supplement users, especially those stacking a multivitamin with other fortified products or high‑retinol foods like liver.
Typical symptoms start subtly: dry skin, brittle nails, headaches, and general fatigue. In the scalp, the excess retinoids disrupt keratinocyte behavior and sebum balance, making strands weaker and more prone to fallout. With prolonged exposure, the shedding can become pronounced—handfuls of hair in the shower or on your pillow.
Animal studies show a consistent pattern: high Vitamin A shortens anagen, accelerates telogen, and reduces hair density. Clinical observations mirror this, with patients recovering once their intake normalizes. It’s not immediate, though. And yes, that part can feel like a very long waiting game.
Thresholds and Risk Factors
Here’s where numbers matter. The recommended daily allowance (RDA) sits at 700 µg RAE for women and 900 µg RAE for men. The upper limit (UL) is about 3,000 µg RAE (~10,000 IU) per day for adults. Chronic intake above this threshold raises the risk of toxicity and hair loss.
Risk factors include:
- Regular liver consumption (even once a week can exceed the RDA).
- High‑dose Vitamin A supplements or certain “skin health” formulas.
- Multivitamins stacked with fortified foods (breakfast cereals, protein shakes).
Provitamin A carotenoids like beta‑carotene are far safer, since the body regulates conversion to retinol. You could eat carrots all day and your hair would likely remain unaffected—though you might look a little sun‑kissed from the carotene pigments.
Is Vitamin A Hair Loss Reversible?
Here’s the hopeful part. Yes, most Vitamin A‑related hair loss is reversible if the excess is corrected. Follicles re‑enter the growth cycle once homeostasis returns, though the timeline varies. Mild cases can see improvement within 2–3 months, while more severe or prolonged exposure may take six months or more for visible density recovery.
Professional evaluation speeds this process. A trichologist or dermatologist will assess dietary history, supplement intake, and may run supportive tests. Adjusting intake, pausing supplements, and supporting hair cycle recovery (for instance, with Laser Phototherapy) can all help restore balance.
How to Tell if Hair Loss is Linked to Vitamin A
So, how can you actually know if Vitamin A is the culprit? That’s trickier than most assume. Hair loss rarely comes with a neat little label saying, “Excess Vitamin A did this.”
First, look at your intake history. Are you on a multivitamin? Eating fortified foods daily? Taking an “anti‑aging” or “skin health” supplement that lists retinyl palmitate or retinol? Even moderate stacking can push levels past the upper limit without realizing it.
Second, examine the pattern of hair loss. Vitamin A excess tends to cause diffuse shedding—evenly distributed thinning rather than isolated bald spots. It often mimics telogen effluvium from stress or illness, which is why professional insight matters.
Blood tests exist, but serum retinol isn’t always reliable. Vitamin A is stored in the liver, so normal blood levels don’t necessarily rule out chronic excess. Clinicians often rely on dietary assessment plus symptom patterns—dry skin, brittle nails, mild headaches, sometimes even joint pain.
If all this feels complicated… it is. And self‑diagnosis is risky. A dermatologist or certified trichologist can guide you through testing and, if needed, a careful tapering of supplements. The upside is that identifying and correcting a nutrient imbalance early can prevent more significant follicle stress and speed recovery.
Safe Intake and Prevention of Vitamin A‑Related Hair Loss
Avoiding this type of hair loss is, thankfully, simpler than fixing it. The key is moderation.
How to Maintain Optimal Levels
Rely primarily on whole foods. A mix of colorful vegetables, occasional dairy, and lean meats provides all the Vitamin A most adults need. Carotenoid‑rich produce (carrots, sweet potatoes, spinach, and kale) offers a natural safeguard because your body converts only what it requires.
Save preformed retinol (supplements, liver) for when it’s truly needed. If you enjoy liver occasionally, limit portions to avoid overloading your stores.
Tips for Supplement Users
-
Read every label—multivitamins, “beauty blends,” protein shakes, and cereals can all contain added Vitamin A.
- Stick to the RDA range unless under medical supervision.
- Avoid doubling up on different products with overlapping doses.
For those recovering from excess intake, patience and monitoring are essential. Professional oversight ensures your levels normalize safely without swinging toward deficiency.
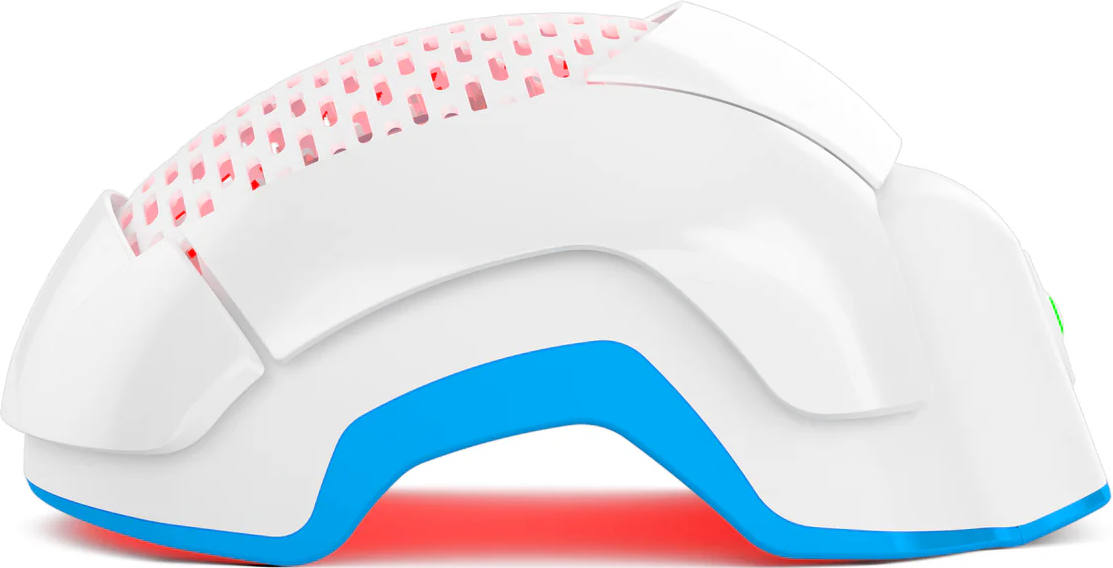
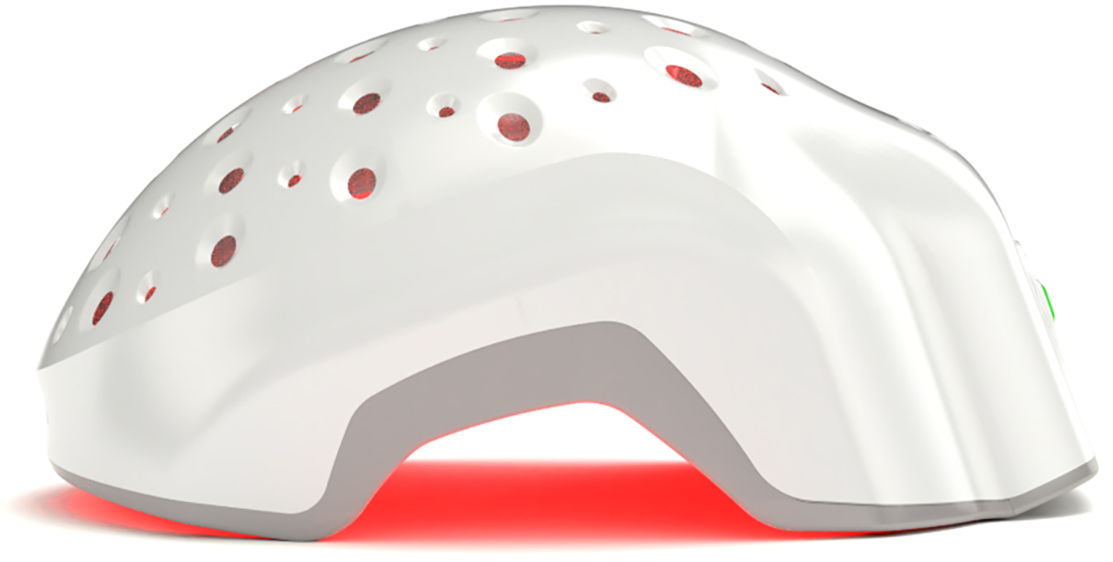
This is also the stage where hair support therapies can play a meaningful role. While nutritional balance lays the foundation, some follicles need a gentle nudge to exit their resting phase. Clinically tested Laser Phototherapy (LPT) devices, like FDA‑cleared Theradome, can stimulate follicles and complement recovery—particularly after telogen effluvium caused by nutrient imbalance.
By respecting intake limits, leaning on plant‑based sources, and seeking professional guidance, most people can keep Vitamin A working for their hair, not against it.
Evidence‑Based Hair Restoration Support
Correcting Vitamin A intake is the first step, but let’s be honest—waiting for hair to bounce back can feel like watching paint dry. Follicles have their own rhythm, and once they’ve slipped into telogen, they don’t just spring back overnight. This is where modern, evidence‑based hair restoration tools step into the picture.
One of the most clinically validated methods is Laser Phototherapy (LPT). Unlike the “hot” lasers you might associate with surgeries or sci‑fi, LPT uses cold, low‑power light that stimulates follicles through a process called photobiostimulation. Essentially, the light penetrates the scalp, energizes cellular activity, and nudges dormant follicles back toward the anagen (growth) phase.
Here’s the interesting bit: multiple studies, including meta‑analyses, confirm that LPT can improve hair density and slow shedding in conditions like telogen effluvium and androgenetic alopecia. And it does so without causing heat damage or scalp irritation. It’s like a gentle push (more of a whisper than a shout) to remind follicles it’s time to work again.
Devices like Theradome make LPT accessible at home. It’s FDA‑cleared, wearable, and delivers full‑scalp coverage with a high dose of safe light energy. For someone recovering from Vitamin A‑related shedding, LPT can serve as the bridge between nutritional correction and visible regrowth, accelerating the return to fuller hair.
Conclusion
If there’s one lesson here, it’s that balance is everything. Vitamin A is essential for healthy hair, but both deficiency and excess can throw your follicles off course. Too little can leave hair brittle and lifeless; too much can trigger diffuse shedding that feels alarmingly fast.
Before you self‑diagnose or toss every supplement in your cabinet, pause. Evaluate your diet. Check labels on multivitamins and fortified foods. Consider whether you might be stacking doses without realizing it. And if shedding persists or worsens, seek a dermatologist or trichologist—they can help identify the root cause and guide safe adjustments.
Correcting intake usually reverses the problem, but patience is required. Hair regrowth may take 2–6 months, depending on how long the imbalance persisted. Supportive strategies, like Laser Phototherapy, can help shorten the recovery gap and give follicles that extra nudge back toward growth.
So, yes—Vitamin A can affect hair in profound ways. But with informed choices, professional guidance, and a bit of science on your side, you can keep your strands strong without crossing the line into danger.