A hair transplant is not the finish line. It’s the handoff.
What happens in the first 7, 30, and 90 days after surgery determines whether grafts settle in calmly, whether surrounding hair panics and sheds, and whether the final result ages well… or starts looking thin again sooner than expected.
One of the most unsettling parts of recovery is shock loss. Not because it’s rare, but because no one enjoys watching hair fall out right after paying to put hair back in.
Shock loss is usually temporary. But how severe it becomes, and how well native hair rebounds, depends less on luck and more on how much physiological stress the scalp experiences during recovery.
This guide lays out a realistic recovery timeline, what the scalp is dealing with at each stage, and how non-contact laser phototherapy (LPT) can be layered in thoughtfully, without touching grafts or turning recovery into a science experiment.
Shock Loss Is Stress-Driven.
After transplantation, two things happen at once:
- Newly placed grafts go through a short period where survival depends on diffusion and gradual reconnection to surrounding tissue
- Nearby, non-transplanted hairs experience inflammation and surgical stress
Some follicles tolerate that stress.
Others don’t.
When susceptible follicles hit their stress threshold, they shift into telogen. That’s shock loss.
Look, it’s not “poor circulation” in the everyday sense. It’s about inflammatory load, cellular energy demand, and how resilient follicles are when the environment changes suddenly.
The best recovery strategy does three things at the same time:
- supports tissue biology without disturbing grafts
- calms inflammation without suppressing healing
- avoids friction, heat, or chemical irritation during fragile phases
Everything else is noise. Just noise.
Where Laser Phototherapy Fits (and Where It Doesn’t)
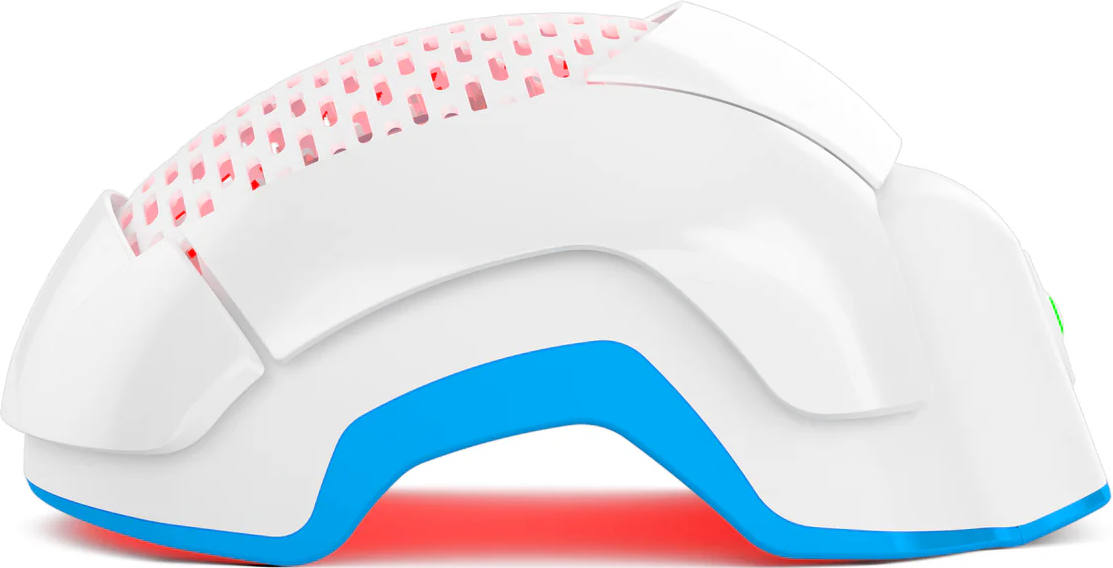
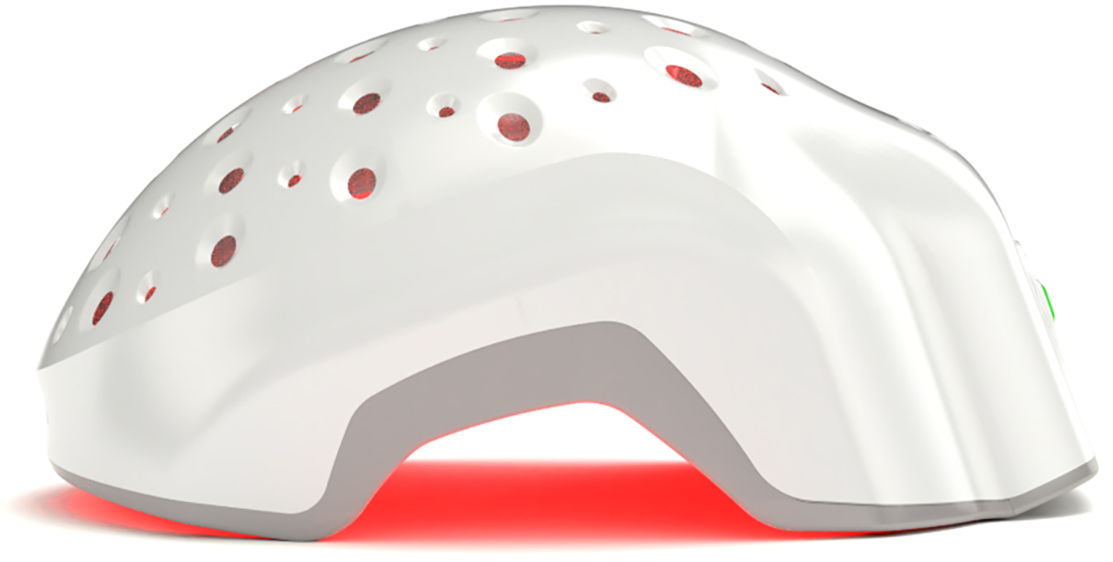
Laser phototherapy, sometimes grouped under low-level laser or photobiomodulation therapy, uses low-power red laser light to interact with scalp tissue biology.
Reviews describe mechanisms such as:
- support of mitochondrial energy production
- modulation of inflammatory signaling
- improved cellular tolerance to stress
Notice what’s missing.
This is not a heat treatment.
It is not a massage substitute.
And it should not be sold as a blood-flow shortcut.
The reason LPT is interesting during post-transplant recovery is simple:
It can be delivered without contact, without friction, and without mechanical disruption, which matters when grafts are settling in and the scalp is reactive.
That’s where device design matters.
A Reality Check on Evidence
There is solid clinical evidence supporting LPT use in androgenetic alopecia, including randomized controlled trials and meta-analyses showing improvements in hair density and shaft thickness versus sham devices.
There is far less direct evidence studying LPT specifically after hair transplantation.
One controlled study using a single LLLT session showed no meaningful effect on transplanted graft outcomes. That doesn’t invalidate LPT. It simply tells us that dose, timing, and consistency matter, and that transplant-specific protocols still need proper study.
So we need to be precise.
The long-term challenge after transplantation isn’t just growing grafts.
It’s protecting the native hair that wasn’t transplanted, because androgenetic alopecia doesn’t politely stop at surgery.
LPT and the Hair Cycle
Why Maintenance Still Matters After Surgery
Multiple peer-reviewed reviews describe LPT as influencing the hair cycle by:
- helping telogen follicles re-enter anagen
- potentially supporting longer anagen duration
That’s why LPT is often positioned as maintenance therapy, not a one-off intervention.
So, using LPT consistently after a transplant may help reduce continued miniaturization of surrounding native hair, which is one of the main reasons patients seek additional procedures later.
Important distinction:
-
Supported by evidence: LPT can improve hair density and is associated with anagen support in AGA
-
Not proven: that LPT guarantees a specific delay before another transplant or reduces the number of future procedures
Any claim about “how many years” a transplant will last crosses from science into storytelling.
We don’t do that here.
The 0–90 Day Hair Transplant Recovery Timeline
What the Scalp Is Actually Doing
Day 0
Grafts placed.
Avoid pressure, heat, friction. Full stop.
Days 1–2
Inflammation peaks.
Grafts rely on diffusion.
Native hairs are vulnerable to stress.
With surgeon approval, non-contact LPT can be introduced gently to support cellular energy and reduce inflammatory burden, particularly for surrounding native hair.
Avoid: vigorous washing, massage, heat exposure, strong topicals.
Days 3–7 (Critical Phase)
Grafts begin establishing tissue connections.
Angiogenic signaling increases.
Scalp sensitivity is still high.
Consistency matters here. Not intensity.
Continue gentle, non-contact LPT if approved.
Avoid scratching or mechanical irritation.
Days 7–14
Swelling and redness settle.
Tissue remodeling begins.
LPT can now be used more routinely across recipient and donor zones to support recovery and native hair stability.
This is a good moment to ask your surgeon when or if to reintroduce topical actives.
Days 15–30
This is the classic shock-loss window.
Transplanted shafts often shed. That’s normal.
Native hair may shed if stress thresholds were exceeded earlier.
Consistent LPT during this phase is about damage control, not acceleration.
Days 31–90
Microvascular structure matures.
Follicles begin re-entering growth.
Early regrowth may appear, slowly.
LPT continues as a foundation therapy. Adjuncts can be layered in if clinically appropriate.
Beyond 90 Days
Density improves gradually over months.
AGA remains the long-term risk.
This is where maintenance separates outcomes that age well from outcomes that thin again.
Conclusion
Shock loss after hair transplantation is common. It’s driven by inflammatory stress and how well follicles tolerate disruption.
A Theradome-first approach focuses on non-contact support of scalp biology during early recovery, followed by consistent long-term maintenance aimed at protecting native hair.
This approach may plausibly reduce the likelihood of needing another procedure soon, not by guaranteeing outcomes, but by reducing ongoing follicular stress and slowing AGA-related thinning.
How long a transplant lasts still depends on genetics, overall treatment adherence, and time.
There are no shortcuts.
But there are smarter defaults.