Accurate diagnosis of hair loss hinges on combining your history + clinical exam + noninvasive tests (pulls, trichoscopy, lab work) and (if needed) a scalp biopsy. These steps allow a trichologist or dermatologist to distinguish between reversible shedding, pattern loss, autoimmune alopecias, or scarring conditions.
Understanding Hair Loss Before Testing
First: not every hair on your brush means something’s wrong.
We lose about 50 to 100 hairs per day as part of a normal cycle (anagen → catagen → telogen).
What matters is the pattern, rate, and persistence—not the occasional strand.
Hair loss may be temporary (telogen effluvium), patterned (androgenetic alopecia), or even scarring (lichen planopilaris, CCCA). The job of diagnosis is to tease apart those possibilities before jumping to treatments.
Measuring the Level of Hair Loss
Before you poke, pull, or microscope your scalp… you’ve got to first see what you’re working with. Literally.
The level of hair loss isn’t just a “gut feeling” or based on how often you’re sweeping the bathroom floor. Clinicians lean on visual grading scales—tools like the Hamilton-Norwood Scale (for men) and the Ludwig–Savin Scale (for women)—to map the pattern, extent, and severity of loss. These are not just charts; they’re the GPS for your diagnosis.
For Men: Hamilton-Norwood Scale
This scale has been the gold standard for male pattern hair loss (MPHL) since the 1950s. It maps seven stages of recession, starting with minor hairline dips (Stage I) to the infamous “horseshoe pattern” (Stage VII).
- Stage I–II: Minor temple thinning. Often unnoticed unless you’ve got eagle eyes or compare old selfies.
- Stage III–V: Forehead and crown become noticeably sparse. Hair may separate into islands.
-
Stage VI–VII: The bridge disappears. Crown and temples merge. Transplants are usually needed here.
Once you’ve hit Stage V and beyond, spontaneous regrowth is unlikely. Intervention gets harder, not impossible—but don’t bet on a shampoo alone.
For Women: Ludwig–Savin Scale
Women’s hair loss doesn’t follow the same script. Instead of retreating temples, you’ll usually see diffuse thinning at the part line that widens over time—like a creek slowly becoming a river.
- I–1 to I–4: Early stages—visible thinning, especially under harsh lighting.
- II–1 to II–2: Moderate expansion of the part line.
-
III and Advanced: Severe loss, often resistant to non-prescription treatments.
The ponytail trick is an underrated red flag: if you find yourself needing to wrap the hair tie more times than last month (using the same band, mind you), you’re probably thinning.
These scales don’t replace a trichologist’s judgment—but they objectively anchor what’s happening on your head. So yes, we love them.
The 12 Clinical Methods to Diagnose Hair Loss (As Used by Experts)
Hair loss is one of the few conditions where patients often walk in already assuming the diagnosis — “I’m shedding, so it must be genetics” — without realizing just how many variables can drive it. That's why trichologists and hair restoration physicians don’t rely on guesswork, patch tests, or TikTok “strands in the drain” tricks. They use a series of clinical hair loss tests designed to rule in (or out) the real cause and guide effective treatment.
Here are the 12 most clinically validated methods used today:
1. Medical & Lifestyle History
Everything starts here. A proper diagnostic process begins with a full picture of the patient’s internal and external environment — including their medical background, hormonal status, lifestyle, stress exposure, dietary habits, and sudden weight changes.
Why? Because hair follicles are incredibly sensitive to internal shifts. Crash diets, post-infection stress, iron deficiency, PCOS, thyroid fluctuations, and medications (like isotretinoin or SSRIs) can all show up in the scalp before they do in a blood test.
2. Visual Pattern Recognition (Hair Loss Mapping)
Before any microscope is pulled out, trained professionals rely on clinical grading scales to assess pattern, progression, and severity.
- Hamilton–Norwood Scale: Used for men; outlines 7 stages of Male Pattern Hair Loss (MPHL), from mild temple recession to full crown exposure.
-
Ludwig–Savin Scale: For women; starts with central thinning at the part line and expands outward, sometimes reaching diffuse or frontal loss.
These scales are key to identifying whether hair loss is androgenic or due to something else (like traction, alopecia areata, or TE).
3. Scalp & Follicle Observation (Trichoscopy)
Using a dermatoscope or digital trichoscope, this non-invasive tool magnifies the scalp and hair shafts 20–70x to evaluate:
- Miniaturization (short, wispy hairs)
- Follicular dropout (spaces where follicles have closed off)
- Redness, scaling, or perifollicular discoloration
- Diameter variation (key for androgenetic loss)
This tool helps differentiate between telogen effluvium, alopecia areata, and androgenic alopecia within minutes.
4. Pull Test
One of the simplest and fastest hair analysis methods. The clinician gently pulls on a small group of hairs (typically 40–60) from different parts of the scalp. If more than 2–3 hairs come out consistently, it may indicate active shedding, such as telogen effluvium.
Important: The test only shows what's happening right now, not cumulative loss.
5. Tug Test
Not to be confused with the pull test, the tug test checks for fragility and shaft breakage. The practitioner holds the hair at both ends and gently pulls in opposite directions to see if breakage occurs. Useful in identifying structural weakness, often due to over-processing, nutritional deficiencies, or certain scalp conditions.
6. Phototrichogram
This digital technique tracks hair growth, density, and cycle phase. After clipping a small patch of scalp, the area is photographed and measured over several days to calculate:
- Hair growth rate
- Percentage of hairs in the anagen (growth) vs telogen (resting) phase
- Changes in hair diameter or density over time
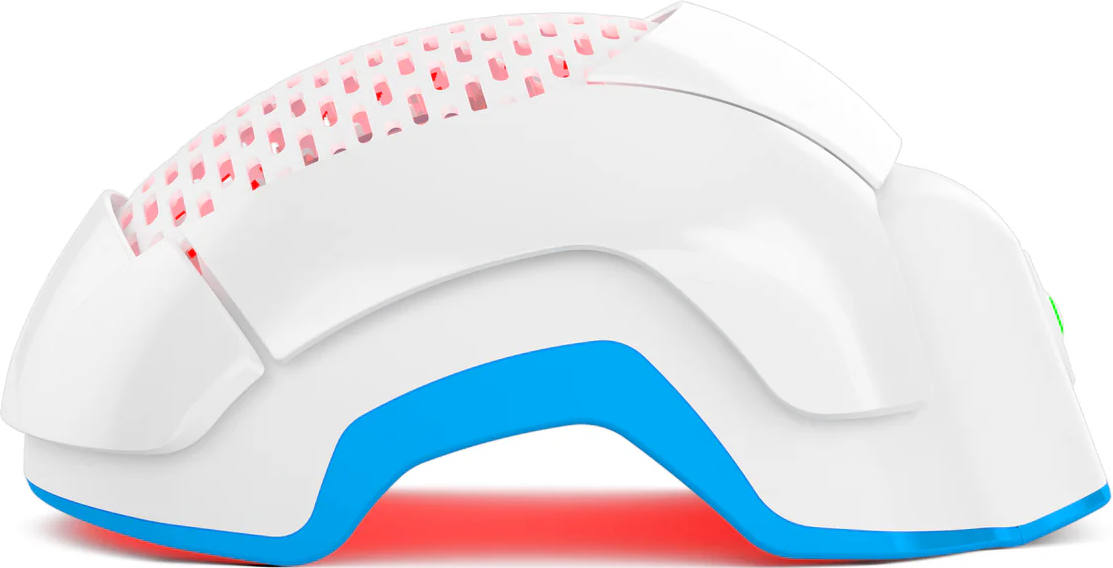
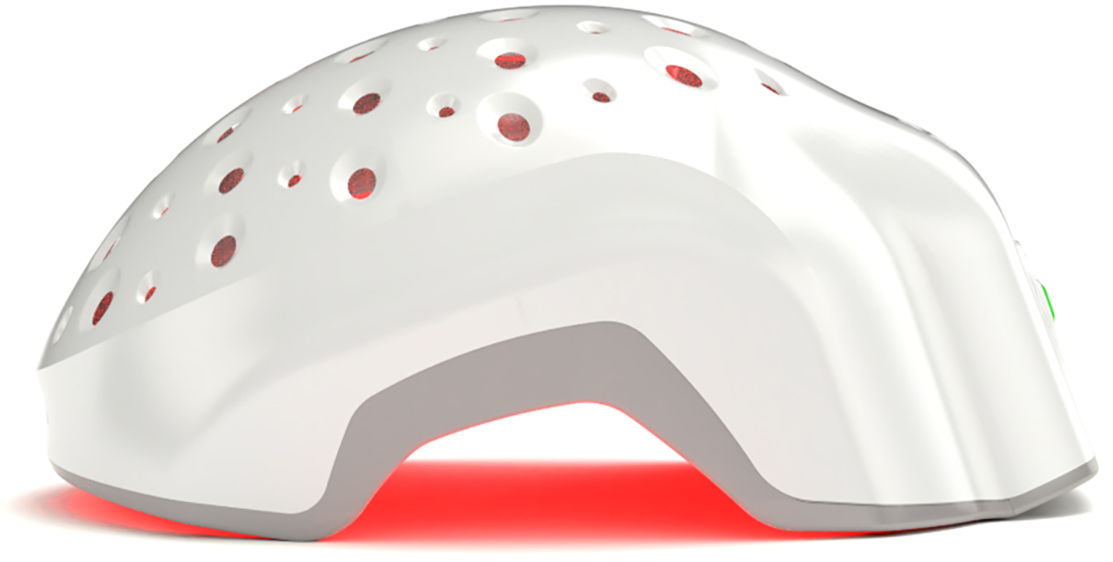
Clinics use it to monitor treatment progress — especially when testing topicals or LPT devices.
7. Global Photography
Not as scientific, but absolutely useful. Standardized before-and-after scalp photography — with consistent lighting, angles, and backgrounds — helps track progress and identify patterns over time. This is particularly helpful for long-term monitoring and documenting subtle density changes the patient may miss.
8. Scalp Biopsy
When the diagnosis is unclear or scarring alopecia is suspected, a scalp biopsy is essential. A small punch biopsy (typically 4mm) is taken and examined under a microscope.
Biopsies help identify:
- Lichen planopilaris (LPP)
- Central centrifugal cicatricial alopecia (CCCA)
- Discoid lupus erythematosus (DLE)
- Follicular inflammation, fibrosis, or absence
So when in doubt, cut it out (gently, of course).
9. Blood Tests
Hair loss is often a symptom of deeper dysfunction. Bloodwork offers insight into internal imbalances, especially for female patients or anyone experiencing sudden or diffuse thinning.
Typical panels include:
- Ferritin (iron stores)
- Vitamin D3
- TSH, Free T3, Free T4 (thyroid function)
- Testosterone, DHEA, DHT
- SHBG (hormone-binding capacity)
- Prolactin, Cortisol, B12
⚠️ Quick Note: While online labs offer “hair loss panels,” results without context can mislead. Interpretation matters more than numbers.
10. Wash Test
Also called the “5-day no-wash” method. The patient refrains from shampooing for five days, then washes their hair and collects the shed strands.
The test estimates:
- Average daily shedding
- Whether the shedding is diffuse or localized
- Phase distribution (e.g., hairs not in the growth phase)
Useful for distinguishing TE from early AGA, especially in women.
11. Hair Diameter & Weight Tests
After clipping a measured 1 cm² area of the scalp, hairs are allowed to regrow for 6 weeks and then are clipped, dried, and weighed. This reveals:
- Growth rate
- Thickness
- Diameter consistency
Clinics use this for treatment efficacy (e.g., tracking results from PRP or laser therapy).
12. Hair Count Methods (60-sec, 24hr, Telogen Zone)
These simple tools still play a role in clinical practice, particularly for tracking progress over time:
- 60-Second Test: The patient combs their hair over a contrasting surface for one minute, and the shed hairs are counted.
- 24-Hour Collection: All hairs shed over a day (often post-shower or brushing) are gathered and measured.
-
Telogen Zone Count: Hair is clipped from a standardized 1-inch zone of the scalp, allowed to regrow, and re-clipped at follow-up to compare regrowth and density.
While useful for establishing a baseline and monitoring shedding trends, these tests cannot provide a definitive diagnosis. That’s because they measure quantity, not cause.
These testing methods help determine the average rate of hair loss, but they cannot identify whether the shedding is due to male pattern hair loss (MPHL) or female pattern hair loss (FPHL). Only scalp analysis and bloodwork can provide this level of diagnostic precision. Scalp biopsies, though invasive, allow for microscopic examination of follicular patterns and structural changes. Similarly, blood tests can reveal hormonal imbalances (like elevated DHT or low ferritin) that point toward the root cause.
In clinical practice, that’s what moves the needle. Identifying the underlying disorder, not just confirming that hair is being lost.
Conclusion
Diagnosing hair loss isn’t a magic trick. It’s a deliberate, stepwise process—rooted in observation, magnification, targeted testing, and occasional biopsy.
When done well, it spares wasted time and heartbreak. It gives clarity. It gives direction.
You don’t have to endure confusion or endless product-hopping. Start with truth. Let science guide your next move. Your follicles might just breathe easier knowing someone is finally listening.