Hair loss rarely behaves like a neat little “one-spot” issue. It starts quietly, it stretches, it recruits nearby follicles over months and years… and by the time you’re staring at a clear thin patch, the neighboring zones have usually been “in the process” for a while.
That’s the core reason full-scalp coverage matters. Not because partial devices are “bad” (they’re not automatically bad), but because biology plus human behavior has a habit of punishing patchy, inconsistent exposure.
And yes, we’re talking laser phototherapy (LPT) here, the safe, low-power kind used for hair growth, not surgical lasers. A wearable helmet format is basically a practical answer to a practical question: can you deliver light where you need it, evenly enough, often enough, long enough, without missing half the scalp?
Why Spot Treatment Falls Short
Let’s be fair. Spot treating feels rational. You see thinning at the crown, so you target the crown. You see temples shifting, you chase the temples.
But pattern hair loss (androgenetic alopecia) tends to behave more like a regional condition than a single dot on a map. The “visible area” is often the loudest part of a quieter, wider process.
Androgenetic Alopecia Doesn’t Stay Put
Androgenetic alopecia is driven by progressive follicular miniaturization in susceptible follicles. Over time, hairs cycle shorter, shafts become finer, and density can decline across a broader zone than you initially notice.
Classifications exist for a reason: the typical patterns are predictable enough that dermatology has mapped them for decades, for both men and women. You’ll often see the Hamilton–Norwood framework referenced for men and Ludwig-based approaches for women, with other systems built to describe variations.
So if your thinning “started” at one point, it doesn’t necessarily stay there. That’s the trap.
Hair Loss Is a Scalp-Wide Condition
Even when the pattern looks local, the biology often isn’t. In female pattern hair loss, for example, thinning commonly shows in the midline and crown region with preservation of the frontal hairline, but the underlying susceptibility can involve a wider scalp area than a single strip.
For men, the crown and frontal scalp are frequent “hot spots,” yet classification systems and prevalence data reflect how often patterns expand with time.
That’s why full-scalp thinking tends to be smarter than “only where I’m worried today.”
Manual Devices Create Coverage Gaps
Handheld devices can work for some people, but they come with human realities:
- inconsistent positioning
- skipping areas without noticing
- varying session length depending on mood, time, fatigue
- over-focusing on the “problem area” while missing the surrounding region
And when studies look at home-use light/laser devices overall, they repeatedly point out device variability and parameter variability as major issues in the category.
You don’t need perfect technique forever. You do need something repeatable.
Dose Only Works Where Light Actually Reaches
This is painfully obvious, yet people still trip over it.
Light therapy cannot influence follicles in areas that didn’t receive meaningful exposure. In other words, “a strong session on the crown” doesn’t magically cover the sides or the back of the thinning zone. Photobiomodulation outcomes depend on treatment parameters and delivery.
So, full coverage is, in a way, a “don’t-miss-the-basics” design principle.
What “Full Scalp Coverage” Actually Means
“Full coverage” is a measurable idea with a few parts that matter more than marketing adjectives.
Coverage Is Area + Distribution + Repeatability
A full-scalp coverage helmet should meaningfully address:
-
Area: how much of the scalp gets exposure
-
Distribution: how evenly that exposure is spread
-
Repeatability: whether you can reproduce that exposure session after session without manual guesswork
Devices vary in design and parameters, and that long-term comparisons between devices and sources are still an active need in the evidence base.
So… full coverage isn’t “more lasers.” It’s more reliable delivery to the scalp zones that actually need it.
Uniform Exposure Beats Concentrated Exposure
Photobiomodulation can show a biphasic dose response. Put simply: too little does nothing, but too much can blunt the effect or change it. It’s not a “turn it up and win” system.
This matters because uneven exposure creates uneven dosing. A concentrated hotspot plus neglected areas is not the same as evenly treating a region.
And yes, this is part of why “coverage” is a serious topic.
Helmets Reduce User Error by Design
A wearable helmet tends to remove a bunch of small failure points:
- you’re not chasing angles
- you’re not trying to remember which quadrant you “did last time”
- you’re less likely to shorten sessions randomly
- you’re less likely to miss zones because you got distracted
It’s just behavioral science.
And behavioral science matters because hair growth interventions are slow. If something is annoying, people quietly stop. (The calendar doesn’t care about your intentions.)
How Laser Phototherapy Interacts With Hair Biology
Laser phototherapy for hair sits under the broader umbrella of photobiomodulation. The literature discusses mitochondrial and cellular signaling pathways as plausible mechanisms, while also being clear that the “best” parameters and the full story are still being refined.
Photobiostimulation, Not Heat
Home-use hair devices in this category are typically using low-level red light (often around the 650-680 nm range), intended to stimulate biological responses rather than heat tissue.
A quick reality check: “laser” is just a type of light source. Medical contexts include both tissue-cutting lasers and low-power therapeutic ones. Different instruments, different goals.
Follicles Respond Differently Across the Scalp
Follicles aren’t synchronized. Some are in anagen, some are in catagen, some are in telogen. Even within the same person, there’s variation across scalp regions.
That matters because photobiomodulation-based approaches aren’t like flipping a switch. They interact with biology that’s already mid-process. Broad coverage improves the odds that, over time, you’re regularly exposing the follicles that are actually in a responsive window, rather than gambling on one small area.
Why Coverage Matters More Than Hair Texture
Hair texture is not the primary variable for whether light therapy can be useful. The key issue is whether adequate light reaches scalp tissue consistently across the relevant regions, and whether the treatment parameters are in a biologically helpful range.
So yes, someone with dense hair might need to be more mindful of device fit and usage consistency… but the bigger lever is still coverage and repetition.
Practical Advantages You Feel Over Time
This is where people expect miracles.
No.
What you should expect, if it’s going to help you, is slow, incremental change: reduced shedding for some, improved hair counts/density measures in studies, and better “cosmetic density” over months, not weeks.
Compliance Is the Deal-Breaker
Most hair loss interventions fail in the real world because people don’t stick with them. Not because they’re lazy. Because life is loud.
Wearables can improve compliance by removing friction. You put it on, you do the session, you move on. Less planning. Less fiddling.
And if you’re thinking, “That sounds too simple to matter”… yeah, I get it. But small friction, repeated for months, becomes a cliff. (That’s just how habits work.)
Full Coverage Supports Prevention, Not Just Recovery
Hair loss management is often more effective when you treat earlier stages rather than waiting for severe miniaturization and density loss.
Dermatology references commonly discuss graded patterns and progression, reinforcing that the visible stage often follows earlier change.
So full-scalp exposure can function as a “future-proofing” approach for at-risk zones, not only a reaction to a single thinning patch.
Why People See Patchy Results With Partial Devices
Patchy results can happen for several reasons, but uneven exposure is a straightforward one.
If one region is treated consistently and another is missed or under-treated, outcomes can appear uneven. This is consistent with the broader PBM concept that dose and delivery matter, and that the category still needs more long-term comparative research.
It’s not always “the device failed.”
Sometimes the plan was mismatched to the scalp.
Safety, Regulation, and What FDA-Cleared Actually Means
People get tense when they hear the word “laser.” Understandable.
Let’s calm it down with plain explanations.
FDA-Cleared Devices
For home-use light/laser devices for hair, you will often see FDA-cleared language, typically through the 510(k) pathway. That’s a regulatory process for certain devices, distinct from the way many medications are evaluated and approved.
A concrete example is the FDA device documentation for the Theradome Laser Helmet PRO LH80, which includes intended use/indications information in its publicly available PDF.
Also, the American Academy of Dermatology provides patient-facing guidance noting that laser therapy (low-level laser therapy) may be an option for some types of hair loss, including hereditary hair loss, and it frames it with appropriate caution.
Not a guarantee. A regulated category with defined claims.
Cold Lasers and Real-World Safety
Low-level therapeutic lasers used in these contexts are designed to avoid thermal tissue damage.
And when people worry about eye injury, it helps to separate two ideas:
- staring into a laser beam intentionally is never smart
- low-power visible lasers have a long history of being low-risk when used responsibly, with safety guidance focusing on avoiding intentional exposure
The FDA’s own guidance on laser pointers notes that risk is very small when Class IIIa/IEC Class 3R pointers are used responsibly, while also acknowledging they can be dangerous in misuse contexts.
If you’re using a wearable device as directed, you’re not aiming it around like a pointer. Different use-case. Different risk profile. Still, basic care matters.
Common Mistakes to Avoid
-
Only treating what you can see today. Pattern hair loss often extends beyond the obvious zone.
-
Assuming more exposure automatically equals better results. PBM can show biphasic dose behavior.
-
Switching methods too quickly. Hair cycling is slow, and studies typically measure outcomes over months, not a weekend.
-
Ignoring device variability. Not all home devices are FDA-cleared, and designs/parameters differ.
- Skipping professional guidance when your diagnosis is unclear. Some hair loss is not androgenetic alopecia, and treatment choices depend on the cause.
Where a Full-Coverage Helmet Fits in a Smart Plan
A full-coverage helmet format can make sense when:
- you’re dealing with androgenetic alopecia (male or female pattern hair loss)
- you want a home-use, hands-free option that supports consistent use
- you value even coverage across at-risk regions rather than chasing a single patch
- you’re comparing devices and want the added reassurance of FDA-cleared documentation for indicated uses (when available)
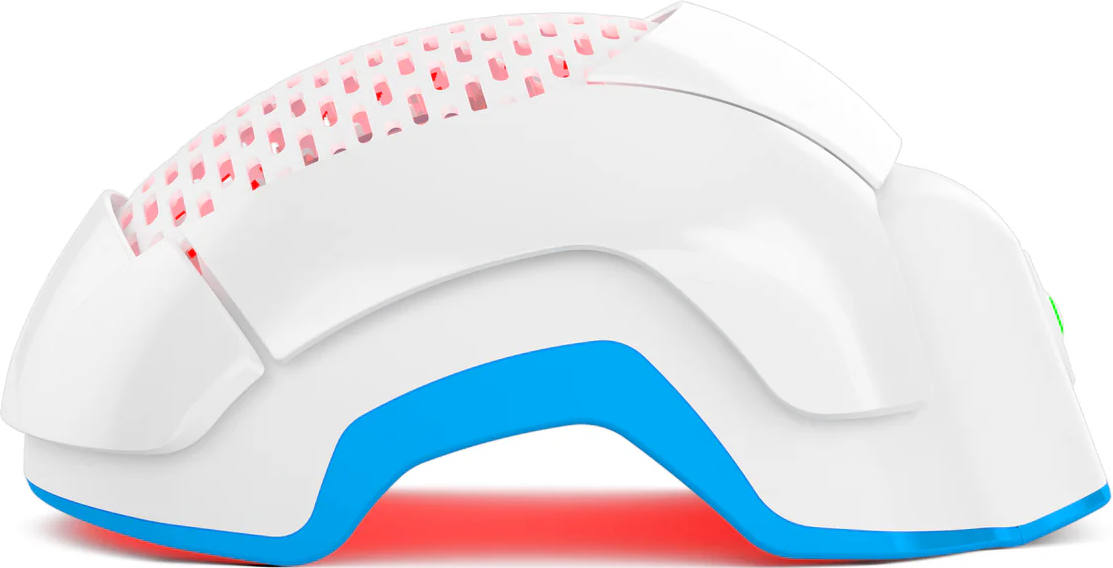
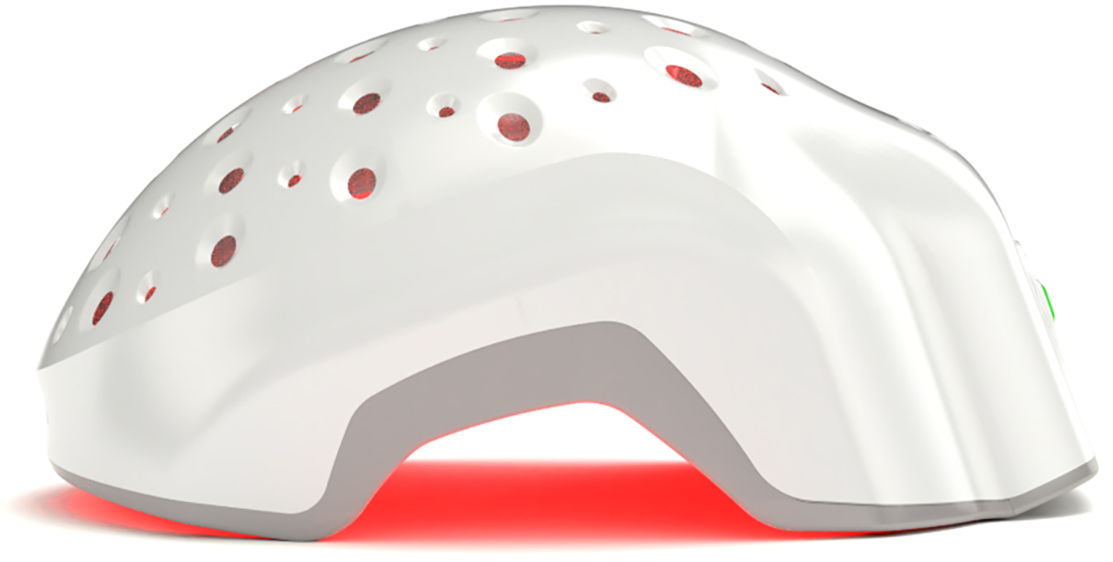
Why Theradome Was Built Around Total Scalp Coverage
Theradome’s helmet structure is built around a simple constraint: if light therapy is going to support follicles across the scalp, the light has to actually reach those areas. To do that, the devices use a fixed array of medical-grade lasers, spaced to cover the scalp evenly rather than concentrating energy in a few spots.
Depending on the model, Theradome helmets use either 80 lasers (PRO) or 40 lasers (EVO), arranged to provide continuous scalp coverage without gaps or overlaps. That spacing is intentional. Uneven delivery can lead to uneven dosing, and with photobiomodulation, consistency matters more than chasing intensity.
The total treatment area is approximately 587 cm², which aligns with the regions typically involved in male and female pattern hair loss. Instead of requiring the user to reposition a device repeatedly, the helmet format keeps placement consistent session to session. Same zones. Same exposure pattern.
From a safety standpoint, the lasers used are classified as cold lasers, meaning they operate at low power levels designed to avoid heat buildup. That allows the device to deliver light across the scalp without creating thermal stress, which is why full-coverage delivery doesn’t automatically mean higher risk.
Theradome was also the first wearable laser phototherapy helmet to receive FDA clearance for the treatment of androgenetic alopecia in both men and women. That clearance reflects how the device delivers light energy within defined parameters for its intended use, not a promise of identical outcomes for every individual.
Taken together, the design isn’t about doing more. It’s about doing the same thing, evenly, every time. For people managing pattern hair loss who want a hands-free option that aligns with how thinning actually spreads across the scalp, that full-coverage approach fits naturally into a broader, evidence-informed plan.
(Which brings us back to the earlier point: coverage plus consistency tends to outperform effort alone.)
Conclusion
Full scalp coverage sounds like a marketing phrase until you treat it like what it is: a practical response to how pattern hair loss behaves and how humans actually stick with routines.
Look, light can only help where it’s delivered, and long-term habits only happen when the process isn’t annoying.
And if you’re weighing options, keep your standards boring and strict: look for regulatory transparency where possible, look for evidence summaries that cite real trials, and pick a format you’ll still be using months from now.
Quiet consistency tends to win.