Hair loss doesn’t just show up to ruin your mirror check—it often shows up as a symptom. And no, it’s not always stress or aging or your pillowcase being too aggressive. There’s a long list of diseases that cause hair loss, and most of them have nothing to do with shampoo. They’re rooted in your biology, your hormones, your immune system, and yes, sometimes even your medicine cabinet.
This blog is not about panicking over every strand in your brush. It’s about decoding what your scalp might be trying to tell you—because when your hair’s acting up, something deeper often is too. Below, you’ll find the real medical reasons hair loss can sneak in, stay too long, and throw off your confidence—and what you can actually do about it.
How Hair Loss Connects to Overall Health
Hair doesn’t just fall out for fun. Every strand grows, rests, and sheds on a tight schedule—unless something interrupts that rhythm. The hair growth cycle (anagen, catagen, telogen) is surprisingly sensitive to internal chaos. Even a small disruption in thyroid hormones, immune function, or nutrient availability can push follicles into “rest mode” prematurely.
And because follicles are among the most metabolically active structures in your body, they’re often the first to react when something’s off. They are the first to be sacrificed when the body is experiencing any inflammation or stress. Hair is, biologically speaking, considered non-essential. That’s why you shouldn’t ignore changes in hair texture, shedding, or thinning. Hair is a biomarker. When it misbehaves, it might be reflecting real health issues happening under the hood.
Medical Conditions That Cause Hair Loss
Hair loss can be the calling card of an underlying disorder.
1. Thyroid Disorders
Both hyperthyroidism and hypothyroidism disrupt the hair cycle. In low thyroid states, hair becomes brittle, sparse, and slow to regrow. In high thyroid states, shedding speeds up and outpaces growth. Either way, the result is noticeable thinning—and it’s often one of the first visible signs of thyroid disease.
2. Autoimmune Diseases
Conditions like alopecia areata and lupus trigger the body’s immune system to attack its own follicles. In alopecia areata, the damage is patchy. In lupus, it’s often more widespread and inflammation-driven. Both are prime examples of autoimmune diseases that cause hair loss—and neither should be shrugged off as cosmetic.
3. Polycystic Ovary Syndrome (PCOS)
PCOS elevates androgen levels in women, which shrinks follicles over time and leads to crown thinning, especially in those genetically predisposed. This is one of the classic presentations of hormonal imbalance hair loss—and treating the hormone issue often makes or breaks regrowth success.
4. Nutritional Deficiencies
Your hair’s hungry for iron, zinc, vitamin D, and protein. Miss one, and the shedding starts. Iron deficiency hair loss is especially common, particularly among menstruating women and vegetarians. It’s a sneaky culprit that’s easy to miss without bloodwork.
Also, you can read our article about how a severe restrictive eating disorder known as Anorexia can affect your hair.
Hormonal Imbalances and Hair Loss
When hormones go rogue, follicles suffer. These are the endocrine issues most commonly caught red-handed.
Androgenetic Alopecia
This hereditary form of hair loss is driven by DHT, a testosterone byproduct that shrinks follicles until they stop producing visible hair. It affects men and women and shows up as receding temples, thinning crowns, or overall density loss.
Postpartum Hair Loss
After childbirth, estrogen levels decrease—and so does hair retention. This temporary shedding (telogen effluvium) often peaks around 3–4 months postpartum and eventually slows, but it catches a lot of new mothers off guard.
Menopause
Reduced estrogen during menopause shifts the hormonal balance in favor of androgens, which leads to gradual thinning. Hair becomes finer, slower to grow, and more prone to shedding. And unlike hot flashes, this one doesn’t always go away.
Medications and Treatments That Cause Hair Loss
Certain medications pull double duty—they treat the condition but also mess with your hair. Medications that cause hair loss include chemotherapy drugs, antidepressants, beta-blockers, anticoagulants, and acne treatments like isotretinoin. These can push follicles into the telogen phase, leading to noticeable shedding within months of starting the drug. It’s called drug-induced telogen effluvium—and it’s more common than most patients are warned about.
Stress & Mental Health Disorders
Chronic Stress
High cortisol levels (your body’s stress hormone) shorten the growth phase of hair and kick more follicles into rest mode. The result is… thinning, shedding, and general volume loss over time. Stress-related hair loss doesn’t happen overnight, but it sneaks up—especially when burnout becomes your baseline.
Depression & Anxiety
Mood disorders alter sleep patterns, nutrition, immune balance, and hormone output. Together, those factors create a perfect storm for disrupted hair cycling. Whether it’s due to poor appetite, low energy, or systemic inflammation, depression and anxiety can tank your hair health—quietly and consistently.
Trichotillomania (Hair-Pulling Disorder)
This is more than a bad habit—it’s a psychiatric condition. People with trichotillomania compulsively pull hair from their scalp, eyebrows, or lashes, often as a response to anxiety. The result is self-inflicted bald spots that can become permanent if not treated early.
Scalp Infections & Skin Disorders
Fungal infections like ringworm (tinea capitis) literally eat away at the follicle, leading to patchy, inflamed bald spots. Conditions like seborrheic dermatitis or psoriasis inflame the scalp, increase skin turnover, and suffocate the follicle’s environment. These scalp infections causing hair loss often go undiagnosed because they mimic dandruff—until the damage becomes visible.
Treatment & Management Options
Treating the cause is always the first move. For thyroid imbalances, you’ll need hormone regulation. For deficiencies, supplementation helps—but only once properly diagnosed. Autoimmune flare-ups may require corticosteroids, immunosuppressants, or even biologics. Infections? Antifungals or antibiotics, depending on the bug involved.
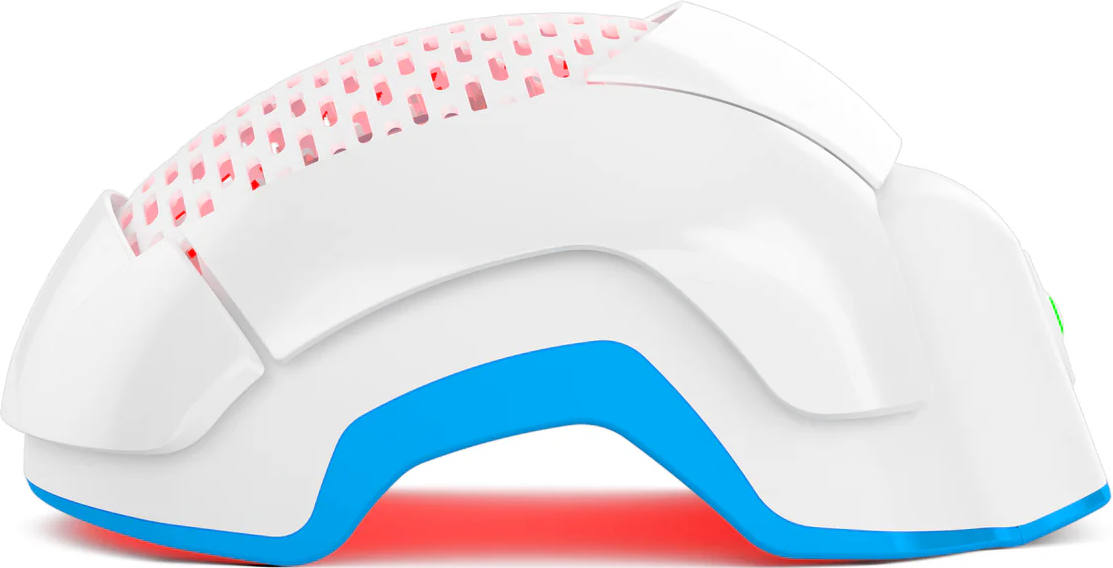
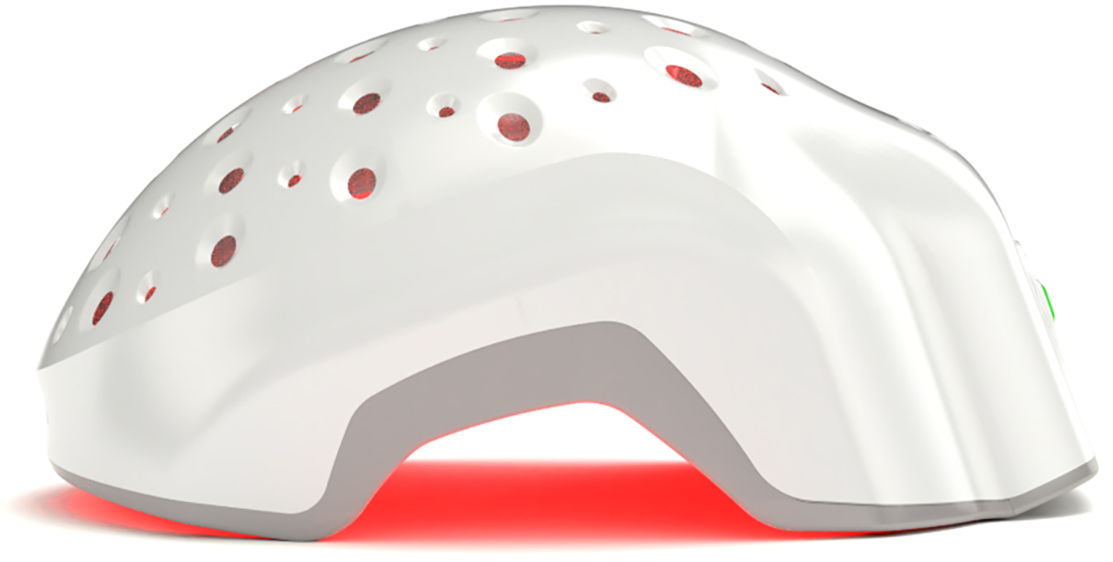
To support regrowth: Minoxidil helps reawaken resting follicles. PRP therapy uses your own platelets to boost regeneration. Laser phototherapy or low-level light therapy like Theradome can improve circulation and follicular function. And if your loss is tied to chronic stress, sleep, movement, and mental health care are mandatory.
Conclusion
Hair loss isn’t always about hair. It’s often about something deeper going off-script inside your body. From autoimmune diseases that cause hair loss to thyroid disease, nutrient gaps, and stress overload, your follicles are signaling systems—not ornaments. The sooner you recognize shedding as a possible warning sign, the sooner you can deal with the root issue. Your hairline isn't gaslighting you. It just might be the most honest part of your health right now.