NASA-Born Technology: Engineering That Never Cut Corners
There is a reason Theradome’s founder obsessed over that VL680 diode. He did not come from the cosmetic gadget space. He came from aerospace.
Tamim Hamid’s Laser Background

Before building hair-growth helmets, Tamim worked as a laser engineer on projects for NASA and related aerospace programs. That work required precision in beam quality, wavelength stability, and thermal behavior that is far above what consumer electronics normally demand.
When photobiomodulation research began to show that specific wavelengths of red and near-infrared light could influence wound healing, tissue repair, and pain modulation, Tamim was already deep into laser work long before hair loss entered the picture.
At the Kennedy Space Center, his focus was not cosmetics or consumer electronics. He was designing and calibrating laser measurement systems for the Space Shuttle’s thermal protection tiles. Precision mattered. Beam stability mattered. Measurement error was not an option. A laser that behaved unpredictably simply was not acceptable in that environment.
Around that same period, Tamim began noticing his own hair thinning. Like many people, he searched for solutions and found the landscape discouraging. Some options were invasive. Others were expensive. Several offered little more than hope. That disconnect pushed him to look at the problem differently, through the lens of biomedical engineering and photonics rather than cosmetics.
Drawing on more than twenty-five years of laser-design experience, he began researching how light could interact with human tissue, particularly hair follicles. That work led him to grow proprietary laser diodes, much like semiconductors, tuned specifically for biological interaction rather than surface illumination. The goal was simple, though not easy: develop a laser device that could reduce hair loss and support regrowth without heat, damage, or risk.
Laser Phototherapy for hair growth is not guesswork here. Theradome has delivered over 110 million at-home treatments with medical-grade cold lasers, across more than 2.2 billion minutes of use, on a device platform that was the first FDA-cleared wearable LPT helmet for androgenetic alopecia in men and women.
Those numbers reflect a huge, real-world dataset sitting on top of solid photobiomodulation science and a very particular kind of engineering obsession.
The Global “Heartbeat” of Hair Regrowth
You know those moments when you are brushing crumbs off your keyboard and thinking about your hairline again. While you read this line, somewhere else on the planet a Theradome session probably just started. That “1 treatment every 3 seconds” rhythm is company-level usage tracking across devices in everyday homes.
110,000,000+ Completed Treatments
Let’s sit with that number for a second.
More than a hundred and ten million sessions means millions of people have strapped on a helmet, hit the button, and sat through twenty minutes of Laser Phototherapy. Not once. Repeatedly. That matters because LPT is a cumulative therapy. Most clinical trials looked at treatment programs over 16 to 26 weeks or more, and hair density gains show up over time rather than overnight.
In those trials, consistent users saw measurable increases in terminal hair counts and hair thickness in androgenetic alopecia, again and again, without serious device-related complications being reported. That is controlled research. Out in the real world, 110 million treatment logs tell us people are, in fact, able to keep going long enough for LPT to have a chance to work.
No device can guarantee that every user gets visible new hair. That would be dishonest. What this scale does show is that adherence is possible and that people tolerate the sessions well enough to keep them in their routine. For a slow, biology-driven therapy, that is half the battle.
1 Treatment Every 3 Seconds
“Once every heartbeat” is the playful way the infographic phrases it, and it is not far off.
A session starts roughly every three seconds across the installed base. That frequency hints at something important we rarely say out loud. People are tired of watching their hair thin. They also prefer treatments that fit around real life, not the other way round.
A helmet you use at home, while scrolling or replying to a late email, removes logistical barriers that clinic-based lasers struggle with. Clinical LPT systems can be powerful, but they also require repeated travel, appointments, and chair time. At-home devices like Theradome shift the bottleneck from “Can I get there?” to “Will I press the button?”. And clearly, a lot of people are pressing the button.
A Legacy Built in 2.2 Billion Minutes of Laser Therapy
If you stack 2.2 billion minutes end to end, you get more than four thousand years of continuous treatment. No breaks. No snack runs.
Turning Minutes Into Meaning
Those 2.2 billion minutes represent countless individual treatment courses: some people using Theradome as monotherapy, others pairing it with minoxidil or prescription medications, many using it as a maintenance tool after seeing early thinning or after hair transplantation. Clinical literature on LPT shows that treatment programs often run for 6 to 12 months or longer before plateauing.
So when you see “4,000 years of continuous therapy” you are essentially looking at a very broad, very long natural experiment in dose tolerance and habit formation. If LPT helmets were uncomfortable, unsafe, or unworkable in day-to-day life, those minutes would never accumulate like that. Usage data does not replace randomized trials but it does support what the trials already showed.
What This Says About Safety
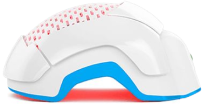
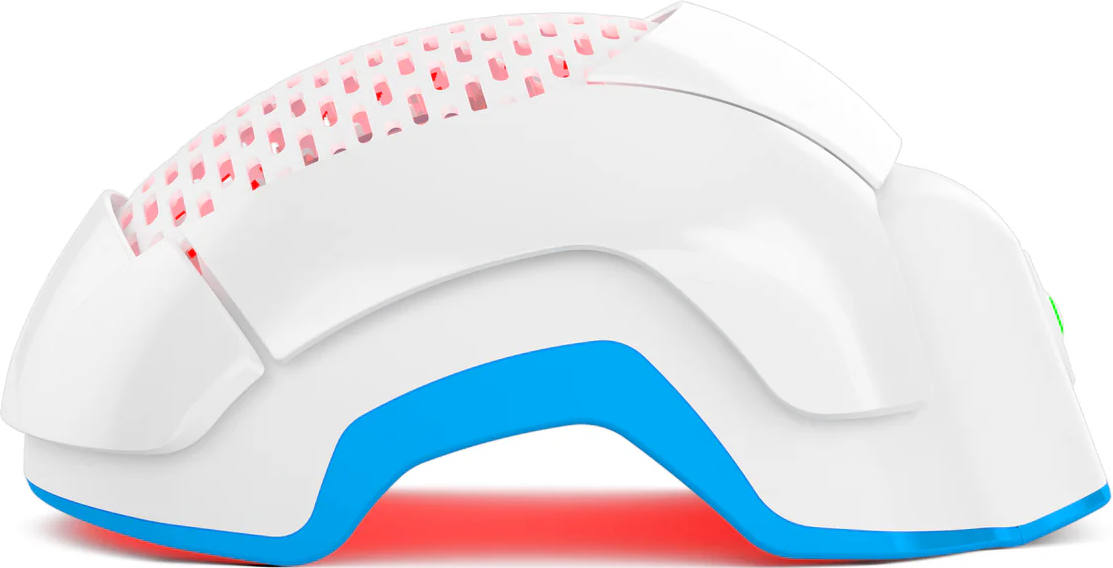
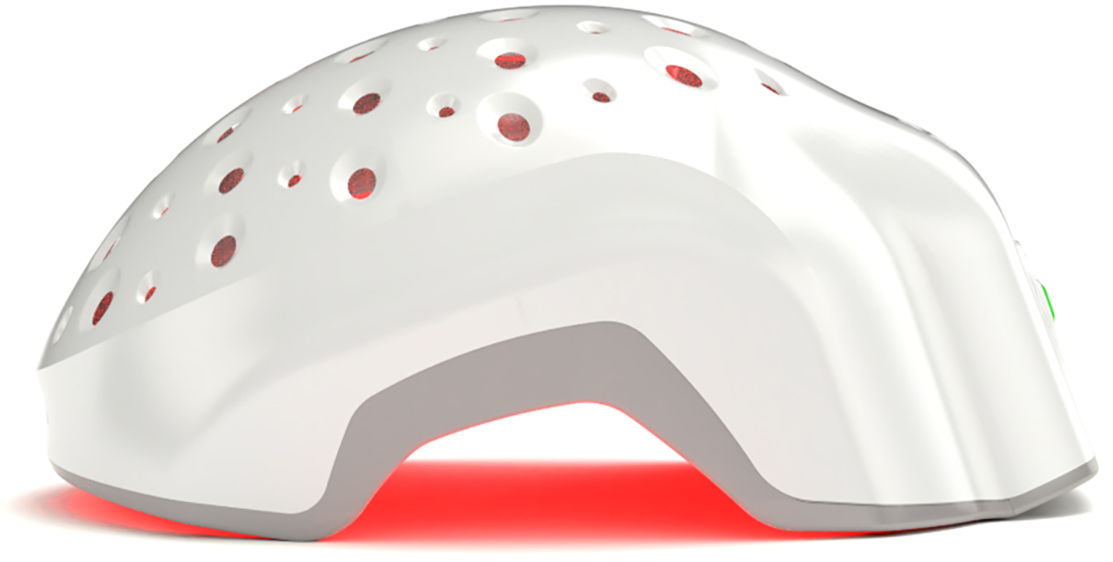
Low-level lasers used in hair devices are “cold” or non-thermal. They sit in the red to near-infrared range and operate at power levels that do not burn skin or heat tissue. Theradome uses Class 3R-level diodes with outputs under 5 mW each and additional safeguards that shut the lasers off when the helmet is not properly seated on the head.
Across multiple LPT trials for androgenetic alopecia, investigators reported no serious device-related adverse events. The most common minor complaints were temporary scalp sensations such as warmth, tightness, or mild itching, which tended to settle without intervention.
Now layer those findings onto billions of treatment minutes in the field. If cold lasers at these parameters were prone to burning skin or causing long-term harm, it would be almost impossible for that amount of use to accumulate without a clear signal in clinical practice and regulatory databases. Instead, we have a therapy that has been repeatedly cleared for at-home use and is still regarded as low risk when used according to instructions.
Why LED Devices Cannot Compete With True Medical Lasers
Let’s talk about the elephant in the treatment cabinet. LED caps are everywhere. They light up. They look science-y. But the way they deliver light into tissue is very different from what a collimated, coherent laser beam does.
LED Devices Scatter; Lasers Penetrate
LEDs emit non-coherent light. The photons fan out, spread, and interact with tissue in a more diffuse way. That is useful for some dermatologic applications at the surface of the skin, but hair follicles sit deeper, around three to five millimeters under the scalp, and they are small. You want energy to arrive there with focus and enough density to matter biologically.
Laser Phototherapy uses coherent beams with a very narrow wavelength band. In Theradome’s case, that is around 680 nm, a range chosen because of how it interacts with mitochondrial chromophores such as cytochrome c oxidase and how it travels through hair-bearing scalp.
So while an LED panel may look bright to the eye, much of that light is lost to scatter and absorption before it gets near the follicle base. The distinction influences dose, and dose is where things get interesting.

One Theradome Laser Helmet Equals To Five Million LEDs
According to Theradome’s internal optical bench testing, each VL680 laser diode in the helmet can deliver roughly 6 joules per square centimeter at the scalp surface over a standard 20-minute session, with sufficient beam quality to carry a meaningful portion of that energy down to follicle depth.
In the same internal comparisons, typical hair-growth LEDs delivered closer to 0.0001 joules per square centimeter at comparable positions, once scatter and divergence were accounted for. One Theradome laser helmet is equivalent to about five million LEDs. It refers to estimated energy density at target depth, not raw device wattage.
These are engineering measurements. The safest way to interpret them is as a reminder that not all “red light on a cap” is equal in terms of dose. If you want to influence mitochondrial activity and cellular signaling in the follicle bulb, the light has to arrive with enough intensity to trigger those photobiomodulation processes in the first place.
Why Dose Beats Diode Count
You will see some devices advertising hundreds of lasers or LEDs. The number can sound impressive. But what matters for tissue is the combination of wavelength, coherence, beam shape, treatment time, and how much energy actually reaches those tiny structures that grow hair.
Theradome’s internal testing suggests that, even when other helmets have more individual diodes, the effective dose delivered at depth can be around 60 to 80 times lower than what the VL680 system produces in a standard session. That gap comes from beam divergence, spacing, and thermal management decisions, not simply “more or fewer lights”.
Those comparisons are best used as context when you are trying to interpret spec sheets that look similar on the surface. In short, the dose that arrives at the follicle matters more than how crowded the dome looks when everything glows red.
The result was a wearable system built to medical standards rather than gadget aesthetics. Power output was deliberately limited to remain in the cold-laser range. Wavelength and beam divergence were tightly controlled. Safety interlocks were engineered so the lasers only activate when the device is correctly positioned on the scalp. What emerged was not a flashy light show, but a clinical-grade tool shaped by aerospace discipline and biomedical intent.
Why 680 nm Matters For Hair
Most LPT systems use red light between about 630 and 680 nm or near-infrared light between about 780 and 850 nm. Those windows are sometimes called “optical therapeutic windows” because light can travel through skin and soft tissue there with less absorption by water and hemoglobin.
Theradome’s 680 nm lasers sit toward the upper end of the red band. At that range, photons are strongly absorbed by cytochrome c oxidase in mitochondria, which is one of the key chromophores in photobiomodulation models. When that enzyme absorbs light under the right conditions, it can kick off a cascade that increases ATP production, modulates reactive oxygen species, and changes transcription factors linked to cell survival and growth.
In hair follicles, those shifts appear to encourage more follicles to enter and remain in anagen, the active growth phase, and may help recover some miniaturized follicles before they are lost. That is the biological backdrop behind that glowing helmet in your bathroom.
50 Million+ Medical-Grade Lasers Deployed Globally
At first, “50 million lasers” sounds like the plot of a science-fiction movie. In practice, it is a count of how many individual medical-grade diodes Theradome has produced and placed into helmets.
What “50 Million Lasers” Actually Means
Each Theradome PRO helmet contains up to 80 proprietary VL680 diodes. The EVO model carries 40. Across years of production, sales, and servicing, those add up. This tally matters because each diode is a tiny, repeatable energy source with known characteristics. The more of them in circulation, the more real-world performance data the company can gather about durability, behavior over time, and usage patterns in different hair types and lifestyles.
Compared with some brands that rely on generic off-the-shelf lasers or LEDs from multiple suppliers, Theradome’s approach is closer to a controlled ecosystem. Same diode family. Same wavelength. Same safety thresholds. That consistency is valuable in a medical-adjacent device.
PRO vs EVO: Dose Density Options
Both Theradome PRO LH80 and Theradome EVO LH40 use the same wavelength and cold-laser principles. The difference is dose density and schedule.
Theradome PRO LH80
- 80 lasers
- high density of 680 nm coverage
- typically used twice per week for 20 minutes
Theradome EVO LH40
- 40 lasers
- slimmer internal array
- usually scheduled four times per week for 20 minutes
Total weekly dose ends up in a similar range, but the pattern is different. Some users prefer fewer, more intense sessions; others like shorter gaps between them. In both models, the emphasis stays on reaching therapeutic energy thresholds at follicle level while protecting tissue from heat.
Leading in Laser Hair Growth: Why Theradome Holds the Top Spot
“Number one” can mean a lot of vague things, so let’s keep it concrete.
Category Leadership With Clear Boundaries
Theradome’s claim to leadership rests on several measurable pillars:
-
First FDA-cleared wearable laser phototherapy helmet for androgenetic alopecia in both men and women.
-
Proprietary VL680 lasers designed specifically for human scalp tissue, not repurposed LED arrays.
-
More than 110 million completed treatments and 2.2 billion minutes of therapy, which is a depth of real-world usage rare in this niche.
-
Strong safety profile consistent with broader LPT literature that shows no serious device-related adverse events in trials.
-
Documented clinical benefit in a randomized, sham-controlled study of the LH80 model, where users saw statistically significant improvements in hair parameters compared with sham treatment.
That does not mean Theradome cures baldness or that other reputable LPT devices have no value. It means that, taken together, engineering design, regulatory milestones, and real-world data place this helmet in a leading position among at-home Laser Phototherapy options.
Answering Your Questions
People rarely start by asking about joules per square centimeter. They want to know simpler things:
- “Will this help my kind of hair loss?”
- “How long before I notice anything?”
- “Is this safe on my scalp type?”
Clinical data tell us LPT works best for androgenetic alopecia in its earlier to moderate stages, when follicles are still alive but producing thinner, shorter hair. Most users who respond notice slowing of shedding and fuller-looking hair over 4 to 6 months and more obvious gains over 6 to 12 months.
As for safety, cold-laser LPT has one of the gentler side-effect profiles in the hair-loss treatment toolbox, especially compared with systemic medications that can affect hormones. That said, anyone with more complex scalp disease, a history of skin cancer, or concurrent systemic illness should involve a dermatologist or trichologist before starting.
How To Interpret These Numbers For Your Own Hair
All of these statistics can feel abstract when you are the one fishing more hairs out of the shower drain. So what do they mean for one person standing in front of a mirror.
First, they tell you that Laser Phototherapy is not experimental vaporware. It has been studied in randomized trials and used in real households for years, with measurable improvement in hair density for many people and a strong safety margin.
Second, they show that the specific way a device delivers light matters. A helmet that has logged 2.2 billion minutes of cold-laser usage with a known dose profile gives you a different level of confidence than an untested LED cap ordered on a whim.
Third, they quietly remind you of the boring truth at the core of all hair-loss management. Consistency often beats intensity. A beautifully engineered helmet sitting in a box does nothing. One that joins your weekly routine, alongside any topical or systemic treatments your clinician recommends, has a chance to support healthier hair behavior over time.
Conclusion
Laser Phototherapy is not magic. It is targeted light interacting with cellular machinery inside hair follicles. When you deliver enough of that light at the right wavelength, for long enough, some follicles behave differently. Clinical trials and real-world use both support that idea.
Theradome takes that underlying science and layers it with aerospace-grade engineering, a wavelength selected for scalp tissue, and an unusually large body of usage data. Numbers such as 110 million sessions and 2.2 billion minutes carry weight because they sit on top of careful design and regulatory scrutiny, not instead of them.
If you are dealing with androgenetic alopecia and looking for a low-risk, home-based option to sit alongside diagnosis and medical care, those numbers are worth paying attention to. Not as a promise. As a signal that you are stepping into something tried, measured, and deliberately built for the long haul.