Laser Phototherapy (LPT) is not a magic switch, but evidence suggests it can safely accelerate the recovery phase in telogen effluvium by reducing shedding and boosting regrowth… especially when combined with trigger correction and holistic care.
What Is Telogen Effluvium?
Telogen Effluvium (often shortened to TE) is a non-scarring type of diffuse hair shedding that occurs when an abnormally high number of follicles slip prematurely into the telogen, or resting, phase of the hair cycle. Unlike patchy hair loss, this process spreads thinning evenly across the scalp—leaving no bald spots but often creating visible volume loss.
Normally, only about 10% of hair is in telogen at any moment. But in TE, that number can spike to 30%–50%, meaning nearly half the scalp’s hair may be resting—or shedding—simultaneously. It’s a startling shift, one that can make even a healthy head of hair look thinner almost overnight.
And heat is an overlooked culprit. Excessive or repeated exposure to heat (whether from aggressive styling, blow-drying, or external environmental sources) can disrupt follicular balance. When follicles overheat, they react defensively by entering a resting state. Tamim explains this well: hair follicles interpret excessive heat as a kind of shock, triggering telogen effluvium. It’s the same biological reflex that can occur after childbirth, high fever, illness, surgery, medication change, or even extreme psychological stress.
Those “resting” hairs are then nudged out as new anagen hairs push upward: a process that, while technically healthy, can look like alarming loss. TE episodes usually appear two to four months after the stress or trigger. For most people, regrowth follows within six to nine months, though in chronic cases it can linger longer.
There’s also a unique form sometimes seen after hair transplantation: a localized telogen effluvium triggered by surgical trauma or heat exposure. In transplanted zones where no new follicles exist, regrowth may not occur—but for the vast majority of healthy scalps, the hair eventually returns once the underlying stressor fades and follicles re-enter anagen.
Emotionally, TE can be unsettling—watching hair gather on your pillow or in your shower drain never feels “temporary” when it’s happening to you. But physiologically, it is. Given patience, scalp health, and avoidance of repeated heat or hormonal stressors, recovery is the rule, not the exception.
What Triggers Telogen Effluvium?
Understanding why TE happens is vital. Here’s a breakdown of common triggers:
-
Physical stressors: severe illness, high fever, surgery, trauma.
-
Hormonal shifts: postpartum, childbirth, stopping hormonal contraception.
-
Nutritional stress / deficiencies: crash dieting, protein malnutrition, iron deficiency, etc.
-
Medication changes: initiating or stopping drugs (e.g., retinoids, beta blockers, anticoagulants).
-
Thyroid or endocrine disorders.
-
Post-COVID syndrome: increasingly documented.
The lag time is critical: TE typically manifests 2–4 months after the triggering event.
(Yes, that “delay” means many sufferers can’t immediately associate cause with effect.)
How Long Does Telogen Effluvium Last?
In most acute TE cases, hair shedding peaks around month 3 post-trigger and gradually subsides over 6–9 months, with regrowth continuing.
Some residual thinning may linger. But in typical TE, follicles remain viable and regrowth is expected.
Chronic TE is trickier: shedding may persist beyond 6 months, often grudgingly waxing and waning.
TE is usually temporary, but patience is essential.
Do Supplements or Medications Help TE?
This is often where confusion and hype swirl.
-
Biotin: Overrated. Unless someone has a clinically proven deficiency (which is rare), biotin usually doesn’t influence TE. We intentionally deprioritize it.
-
Targeted supplementation: If lab tests show deficiencies (e.g. low ferritin, vitamin B12, hypothyroidism), correcting those may help.
-
Minoxidil: More evidence exists for Androgenetic Alopecia use than TE. Some dermatologists may try it off-label, but it's not standard in classic TE.
-
Lifestyle & stress management: Huge role. Sleep, diet, avoiding further insult, gentle hair care.
In many TE cases, the best “treatment” is stabilizing the system that triggered it and giving follicles time.
What Is Laser Phototherapy (LPT)?
Laser Phototherapy (LPT) is a form of photobiomodulation that uses low-power red/near-infrared light to influence cellular activity without heating or burning tissues.
Key distinctions:
- It’s a cold laser (safe, non-thermal, often <5 mW per diode).
- One of the mechanisms is absorption by mitochondrial cytochrome c oxidase, increasing ATP, nitric oxide (NO) release, and mild signaling that may stimulate growth pathways.
Devices are often FDA-cleared (510(k)), not “approved” in the drug sense. That’s a crucial distinction.
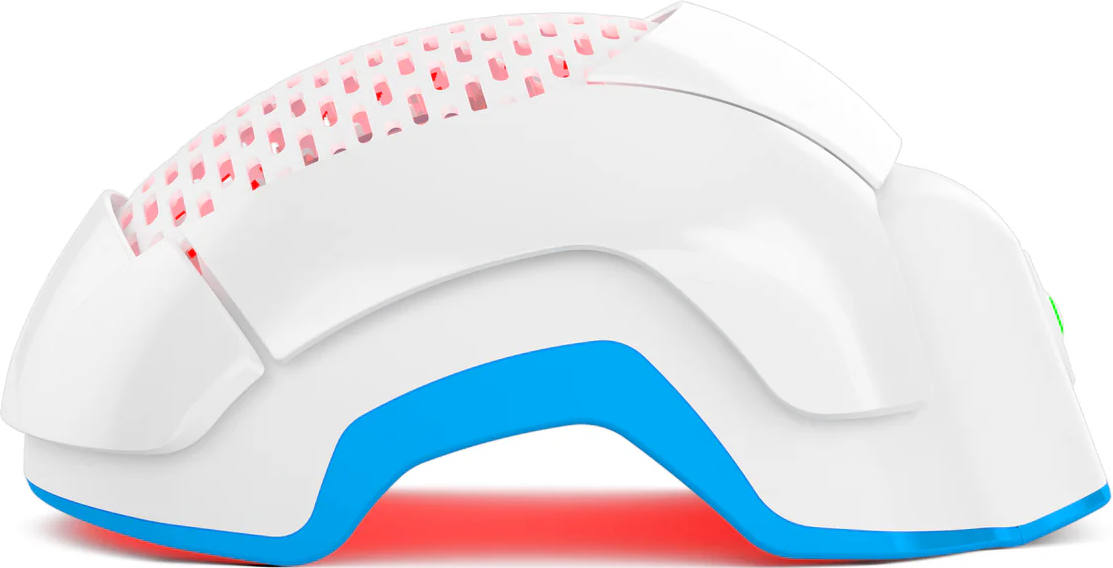
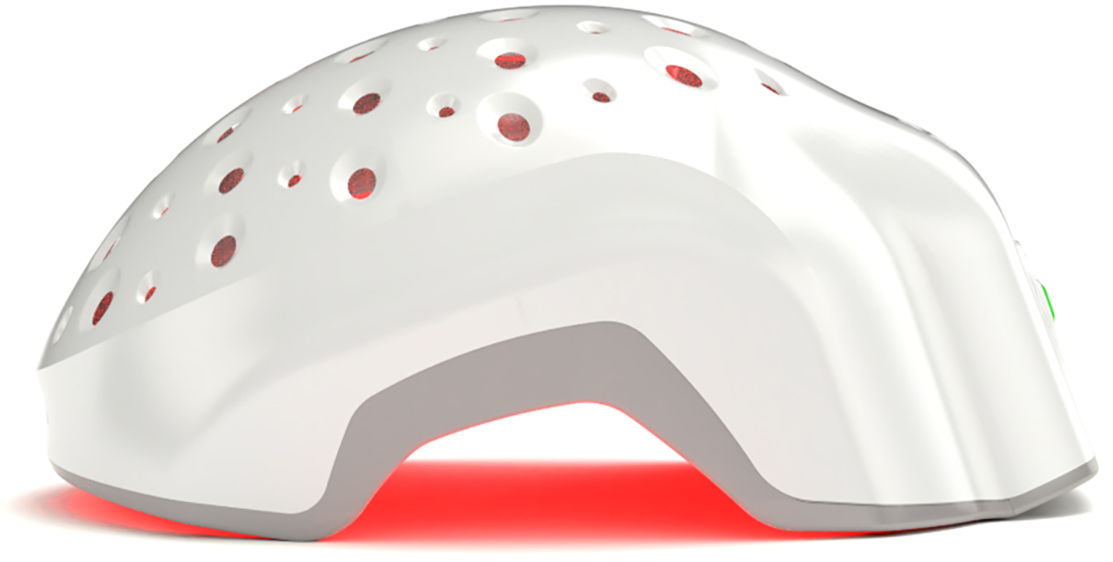
Users benefit from wearable helmets, caps, combs designed for routine use.
Stimulating Follicles Back into Growth Phase
LPT is believed to help push follicles from telogen into anagen earlier—and improve the “vigor” of regrowing follicles.
Enhancing Blood Flow & Nutrient Delivery
The therapy may increase microvascular perfusion, delivering more oxygen, glucose, and growth factors to follicles.
Reducing Inflammation & Cellular Stress
LPT may downregulate pro-inflammatory cytokines, reduce oxidative stress, and create a more favorable biochemical environment.
What Does the Research Say About LPT for TE?
This is the crux — promising but not definitive.
Evidence in AGA / Pattern Hair Loss
Multiple RCTs and meta-analyses demonstrate significant hair density & diameter gains vs sham in pattern hair loss with LPT devices.
For example, one meta-analysis of 7 randomized sham-controlled trials found a standardized mean difference in density of ~1.27 favoring LLLT over sham.
These strong results build confidence in LPT’s mechanism, even if AGA ≠ TE.
TE-Specific / Emerging Data
- A 2024 retrospective LED study in long-COVID TE found that patients receiving LED therapy more often experienced cessation of shedding and improved hair counts relative to controls (p < 0.001).
- However, a 2024 systematic review of laser/phototherapy across alopecia types noted: in some TE studies, no significant change from baseline was observed (lack of strong TE-specific RCT support).
So: biologic plausibility + positive anecdotal/LED data, but no gold-standard RCTs for laser in TE yet.
Limitations & Caveats
- Heterogeneity across device types, light parameters, study durations make generalizing hard.
- Improvements may be confounded by natural TE resolution.
- Sample sizes in TE studies are small.
- LED studies differ from laser devices (beam coherence, depth).
We present LPT as a well-reasoned adjuvant, not a guaranteed cure.
Is Laser Phototherapy Safe for TE Patients?
Yes, within the tested parameter ranges. But let’s discuss the safe and cautious bits.
-
Cold lasers / low-power: These devices typically use Class 3R (≤5 mW per diode), which is nonthermal and generally safe for home use.
-
FDA-cleared devices, not “approved”: Because they are cleared via 510(k) pathways (substantial equivalence), explain the difference to readers.
-
Adverse events observed in trials: mild scalp itching, transient shedding, occasional erythema or headache—nothing severe.
Contraindications / cautions:
- Avoid direct ocular exposure (don’t aim beams into eyes).
- Avoid treating over known malignant scalp lesions or active skin cancers.
- Use caution if on photosensitizing medications or with photosensitive epilepsy.
- Pregnancy/fetal exposure: data limited—consult a clinician.
Proper use as directed is low risk.
Practical Use: How & When to Use LPT for TE?
Because TE is transient and variable, the approach must be nuanced.
- Use protocols validated in AGA trials as baseline (e.g. 20–25 minutes, every other day for 16 weeks) as an analog.
- Start early in the recovery window (when shedding is still active but trigger is stabilized).
- Consistency is key — irregular use will likely blunt effect.
- Combine with trigger correction, nutrition, gentle hair care; don’t expect LPT alone to solve underlying health issues.
- Manage expectations: visible changes may take months, not weeks.
- For men vs women, protocols are largely similar, though demographic response may differ.
Theradome’s Role in Managing TE
This is where Theradome bridges technology and trichology.
When treating TE, precision matters… especially in how a laser device manages heat. Many assume that more lasers equal better results, but that’s a misconception. In reality, more diodes can generate more heat, and heat is not your scalp’s friend. Unchecked heat can irritate follicles and, paradoxically, contribute to the very condition we’re trying to fix—telogen effluvium itself.
That’s where Theradome’s proprietary laser system stands apart. Our engineers designed and tested every diode to emit less than one degree centigrade of heat over a standard twenty-minute session. The goal is to deliver maximum therapeutic energy to the scalp while maintaining ultra-low thermal output. This fine balance ensures effective follicular stimulation without risking heat-related stress.
In simpler terms—more lasers don’t always mean better results; smarter lasers do. The Theradome’s configuration achieves the ideal harmony of dosage and safety, giving follicles the energy they need to re-enter growth without the threat of overheating.
It’s the blueprint for responsible Laser Phototherapy: high dose, low heat, and consistent, comfortable use. When combined with physician guidance, lifestyle optimization, and time, this precision-engineered approach can make the recovery journey for TE smoother—and a bit more hopeful.
Conclusion
Telogen Effluvium is distressing. But in most cases, transient and recoverable if the trigger is addressed.
Laser Phototherapy (LPT), especially via medically cleared helmets like Theradome, offers a safe, scientifically grounded strategy to support regrowth, reduce the shedding window, and provide hope during recovery.
However: results vary, and LPT should be framed as an adjunct… not a magic cure.
If you’re in that shedding phase right now, combining trigger identification, holistic care, medical evaluation, and thoughtful LPT use gives the best odds.