Let’s be honest, your hairline is architecture. Identity. A subconscious signal of age, health, symmetry… and yes, sometimes anxiety.
Most of us don’t think much about our hairline until one day we do. Maybe it’s the mirror lighting at a friend’s house. Or a photo someone tagged you in (you didn’t ask for that angle). Or maybe your partner said something like, “I think your forehead’s bigger than before,” and now you can’t unsee it.
Here’s the truth: hairlines come in many shapes, positions, and textures—and not every shift is something to panic about. But knowing what’s normal, what’s not, and what science-backed options actually help is powerful. And that’s what this guide is for.
We’ll walk through the different types of hairlines in men and women, what causes change (naturally or otherwise) and how to identify the red flags. Then we’ll show you what to do about it, based on real science.
What Exactly Is a Hairline?
You’d think defining a “hairline” would be simple. It's where your forehead ends and your hair begins, right?
Technically, yes—but it’s more anatomical than aesthetic. The true frontal hairline is anchored by a landmark called the trichion… a point just above the glabella (that flat space between your eyebrows). From there, the hairline stretches laterally toward the temporal peaks, which shape the “corners” of the forehead.
Together, these points define the anterior scalp border—where the dense terminal hairs begin. It's also where styling, self-esteem, and (sometimes) stress all meet.
Now, here's where it gets interesting: forehead height and hairline shape differ between sexes, ages, and ethnicities. Most women naturally have a rounded or slightly bell-shaped hairline with more lateral fullness. Men tend to have a flatter or M-shaped hairline with more defined corners—and yes, often a naturally higher set point.
And while the "ideal" ratio between forehead height and facial thirds has been debated in both aesthetic and craniofacial surgery circles, the truth is... there's a wide range of what’s biologically normal.
The problem isn’t just where the hairline is—but how it changes. We’ll get there.
What Are the Common Hairline Types in Men and Women?
Hairlines are like fingerprints. No two are identical. And while they might not show up in crime investigations (unless you’re hiding hair transplants), understanding the different types can tell us a lot—about genetics, aging, and sometimes pathology.
Let’s break them down.
Natural Variation (Non-Pathological)
1. Rounded or Bell-Shaped Hairline
Common in women. The corners curve downward gently, creating a “frame” for the upper face. Soft, youthful, and often low in the center. Like: no harsh corners—just a clean, subtle swoop.
2. Straight Hairline
More frequent in men, though some women have it naturally. The line moves horizontally across the forehead with minimal dip or curvature. It’s not always associated with youth—but it does create a bold, structured look.
3. M-Shaped Hairline
This one gets people panicking. But let’s be clear—not all M-shaped hairlines mean balding. Some men are born with deeper temples, giving the frontal edge that classic "widow’s peak with corners" look. It can be stable for decades.
4. Widow’s Peak
A sharply defined V-shape in the center of the forehead. While Hollywood often turns this into a villainous trope (seriously, check any Disney antagonist), it’s a perfectly normal variant. It doesn’t guarantee recession—it just adds flair.
5. Oval or U-Shaped
Seen often in women with naturally high foreheads. Smooth, curved contours without any distinct peaks or dips. Creates an open look—and often misunderstood as a receding hairline when it’s just a different canvas.
6. Asymmetrical Hairline
Yep, totally common. Most people have slight asymmetry—left vs right differences in temple height or curve. Unless it’s sudden or progressive, this isn’t a cause for concern.
Mature vs Juvenile Hairline (in Men)
Now, this one deserves its own little stage.
Somewhere around the ages of 17–25, many men experience a natural shift from a juvenile to a mature hairline. The corners creep back a bit. The frontal edge rises slightly—often by 1–1.5 cm. It’s part of the hormonal evolution. Testosterone says hello, and your hairline nods respectfully and steps back.
Not a crisis.
Unless... that retreat keeps going. Or gets patchy. Or the temples hollow out aggressively. Then we’re in a different category: androgenetic alopecia (AGA)—which we’ll dive into shortly.
But just because your hairline isn’t where it was at 15 doesn’t mean you’re going bald. (Let’s breathe.)
Ethnic and Ancestral Influence
Hairline shapes can vary across ancestry groups—not as a rule, but as a trend. For example:
- Individuals of East Asian descent often exhibit lower, straighter hairlines.
- African ancestry may be associated with rounded or bell-shaped lines, especially in women.
- European men often develop early temporal recession, sometimes forming pronounced M-shapes even in adolescence.
Texture matters, too. Coily or curly hair tends to obscure the hairline border, especially with natural shrinkage and volume. Straight hair, on the other hand, can expose even the slightest recession under certain lighting. (You know what we mean.)
So, variation is not pathology. Pattern and progression matter more than shape alone.
Is It Concerning If Your Hairline Changes?
Hairlines aren’t static. They shift, breathe, adapt. Sometimes it’s gradual and barely perceptible—like watching a glacier move. Other times, it's more like a landslide (or at least that’s how it feels in the mirror).
But here’s the trick: knowing when change is normal… and when it’s your scalp waving a tiny red flag.
Physiological Shifts (Totally Normal)
Let’s start with the stuff that’s part of the human blueprint.
- Maturation (mostly in men): As covered earlier, the “juvenile to mature hairline” transition is hormonally driven. Usually begins post-puberty and can finish by the mid-20s. The temples recede slightly. The hairline shifts upward maybe a centimeter or so. No shedding. No miniaturization. Just a relocation. It’s not the enemy. It's just a phase.
-
Postpartum (in women): Now, this one can really shake you up. About 2–4 months after giving birth, many women notice sudden shedding—especially around the temples and frontal margin. It’s called postpartum telogen effluvium. It’s like hormonal whiplash. Estrogen drops, follicles freak out. But good news is… most of the time, it rebounds within 6–12 months. Those fine, fluffy “baby hairs” at the front? That’s your scalp rebooting.
-
Menopause & aging: With estrogen declining, some women experience diffuse thinning or notice the frontal “fringe” looks finer. It’s subtle at first. But it’s real. And totally tied to hormonal shifts. (Not your fault. Not your shampoo. Not your pillowcase.)
When It's Not So Innocent
So... when should you raise an eyebrow at your hairline?
- The recession is rapid, not slow.
- There’s visible thinning, not just reshaping.
- You feel itching, burning, or soreness.
- You spot redness, scale, or flaking right at the hairline edge.
- Or—and this one hurts—you’re seeing your eyebrows thin out too.
That’s when the conversation shifts from normal physiology to possible pathology.
Let’s preview a few of the main suspects:
-
Androgenetic Alopecia (AGA): progressive miniaturization; often starts at the temples in men, widening part in women.
-
Frontal Fibrosing Alopecia (FFA): a scarring condition, often misread as “just stress” until it’s too advanced.
-
Traction Alopecia: style-induced loss, common with tight ponytails, braids, wigs.
-
Ophiasis (Alopecia Areata): immune-triggered; band-like loss around the edges.
-
Contact dermatitis or seborrheic dermatitis: flaking, inflammation, and perceived hairline changes.
Each has its own fingerprint. Which is why—yeah—we need to go deeper.
Key Conditions That Alter the Hairline
Hairline changes aren't all created the same. Some scream. Some creep in so quietly you don’t notice until your sunglasses suddenly feel too big.
Now, let’s run through the big five conditions that affect the hairline, their tell-tale signs, and what the evidence says about each.
1. Androgenetic Alopecia (AGA)
Also known as pattern hair loss, this is the most common culprit behind hairline recession in both men and women.
In Men:
- It typically starts at the temples.
- Gradually forms an M-shape.
- Then it marches backward toward the crown.
This isn't just about fewer hairs—it's about miniaturization. The follicles produce finer, shorter, wispier hairs over time. Dermoscopy (aka trichoscopy) will show hair diameter diversity. That’s a dead giveaway.
In Women:
- Often spares the hairline—at least initially.
- More likely to cause widening of the part and diffuse thinning at the crown.
- Some women do experience frontal thinning, especially postmenopausal.
What causes it? Genetics, mostly. And androgens (testosterone and its more potent cousin, DHT).
2. Frontal Fibrosing Alopecia (FFA)
This one's serious. A scarring autoimmune condition that targets the frontal and temporal hairline—sometimes permanently.
Clues:
- A band-like area of recession that looks too clean, too symmetrical.
- Loss of eyebrows (often early).
- Redness, scaling, and follicular dropout seen under trichoscopy.
It mostly affects postmenopausal women, but cases are rising across all groups. The cause? Still under debate—possibly hormonal, possibly environmental, possibly both.
Time is key. This condition doesn’t “pause.” It needs early intervention.
Read more about Frontal Fibrosing Alopecia
3. Traction Alopecia
You might not think of style as a medical issue, but... here we are.
Traction alopecia results from chronic pulling on the frontal and temporal hairs. The culprits are tight ponytails, braids, buns, wigs, headbands, or even repeated use of strong-hold edge control gels.
Signs:
- Thinning along the edges—especially the temples.
- The “fringe sign”: short preserved hairs along the border while the area behind thins out.
The good news is… it’s preventable—and often reversible if caught early. Stop the stress on the follicles, and they usually bounce back.
The bad news is… prolonged tension can cause permanent damage over time.
4. Alopecia Areata (Ophiasis Pattern)
Alopecia Areata is an autoimmune condition that causes sudden, patchy hair loss. The ophiasis variant forms a band-like pattern along the sides and back of the head—sometimes encroaching on the hairline.
This is less common—but important.
Trichoscopy may reveal exclamation point hairs (thinner at the base), yellow dots, or black dots (broken hairs). It’s often triggered by stress, infection, or other immune shifts.
It can resolve spontaneously. But recurrence is common.
Read more about Alopecia Areata
5. Dermatitis Along the Hairline
Last but not least—the imposters.
Conditions like seborrheic dermatitis, psoriasis, or contact dermatitis (from edge gels, adhesives, or helmets) can mimic recession.
They cause:
- Redness
- Scaling
- Flaky buildup
- And sometimes temporary hair shedding
But they’re not truly damaging the follicle—unless left untreated or compounded by scratching, tight styling, or infections.
Diagnosing these requires both eyes and tools: dermoscopy, sometimes biopsy.
So… what do all these have in common?
They affect the frontal margin—that thin, vulnerable border between scalp and face. And while their causes differ, the earlier you identify the pattern, the more options you have to treat it (or halt it entirely).
How to Assess and Track Your Hairline?
You can’t manage what you don’t measure. (And no, squinting at old selfies doesn’t count as data.)
The truth is, most people don’t notice gradual hairline changes until it’s “too late”—or at least until the shift is visible enough to feel like a betrayal. But there’s good news: with a bit of structure and a few smart habits, you can track your hairline the same way a dermatologist or trichologist would.
At-Home Tracking Techniques
1. Standardized Photos (The Gold Standard)
Take a deep breath. Grab your phone. Then follow this:
- Use consistent lighting (no overhead bulbs that exaggerate thinning).
- Keep your hair parted and brushed back (or damp if curly) for clear visibility.
- Take photos from:
- Direct front
- 45° angles from each side
- Top-down (crown view)
- Direct front
- Use a headband or hair clips to expose the hairline without tension.
Repeat monthly. Don’t over-analyze week to week—it’ll drive you mad. You’re looking for patterns over time, not overnight miracles or disasters.
2. Tracing Templates
Old-school? Sure. But it works.
Use a clear plastic sheet or even a transparency film. Place it on your forehead and trace the hairline once a month. Mark the date. Stack and compare. This is surprisingly revealing over a 3–6 month period.
3. The “Mirror Glance Test” (Unreliable, but we all do it)
Just… know that morning lighting, humidity, and hairstyle can all affect how your hairline looks. This one’s more for your gut check than your clinical file.
Clinical Evaluation: What Professionals Look For
If you decide to book a visit (and yes, that’s wise if anything feels off), here’s what your specialist will likely do:
-
Visual Exam: Checking symmetry, density, inflammation, and any signs of follicular dropout.
-
Trichoscopy: This is where science steps in. Using a handheld scope, the clinician looks for:
- Hair shaft miniaturization (AGA)
- Perifollicular redness or scale (FFA or inflammation)
- Yellow dots, exclamation hairs, black dots (Alopecia Areata clues)
- Hair shaft miniaturization (AGA)
-
Medical History: They’ll ask about:
- Family hair loss patterns
- Hormonal shifts
- Recent stressors or illness
- Hair care practices
- Family hair loss patterns
-
Possible Biopsy: If scarring alopecia is suspected, a small punch biopsy may be performed for diagnosis confirmation.
One more thing (and this isn’t a joke): The camera on your phone is more honest than the mirror in your bathroom. Use it. Trust it. Document. Then decide.
Because what feels like sudden change is often slow erosion—and that, thankfully, is still manageable.
Evidence-Based Treatments That Target Hairline Changes
Alright—deep breath.
This is where things get complicated and empowering. Because now we’re not just observing the problem—we’re fighting back, with strategy.
The treatments below are split into tiers—not because one is “better” than the other, but because different approaches work better at different stages, in different people.
And this is critical: the frontal hairline can be slower to respond than the crown. Why? Fewer active follicles. More resistance to regrowth. But it does respond—especially if you catch it early and treat it consistently.
Tier 1: First-Line Treatments
Topical Minoxidil
-
Mechanism: Extends anagen phase (growth), increases follicular size, improves blood flow.
-
Strength: 5% foam or solution
-
Frequency: Once or twice daily
Topical minoxidil has proven efficacy in both men and women. While most studies focused on the crown, real-world dermatology data confirm visible improvement at the temples and frontal edge, especially in early cases.
Oral Low-Dose Minoxidil (LDOM)
- Off-label use; typically 0.25–5mg daily
- More systemic, better for widespread thinning or non-responders to topical
- Risks: Facial hair spillover (vellus), ankle swelling, heart rate elevation in sensitive users
Yes, it’s potent. But it’s not “magic overnight.” Hairline improvements typically show up after 3–6 months, with continued gains over 9–12 months.
Anti-Androgens
For Men: Finasteride (1mg/day)
- FDA-approved
- Blocks conversion of testosterone to DHT
- Proven to slow recession, including frontal zone (yes, it’s been studied)
- Risk: sexual side effects in a small subset; discuss with provider
Read More: Does Finasteride work for hair loss?
For Women: Spironolactone (50–200mg/day)
- Off-label use
- Blocks androgen receptors, lowers DHT
- Especially useful for PCOS or hormonally mediated thinning
- Caution: Not for use in pregnancy. Monitor potassium levels.
Tier 2: Evidence-Based Adjuncts
Microneedling
-
Mechanism: Micro-injury stimulates healing and growth factor release
- Often paired with topical minoxidil (enhances penetration)
-
Frequency: Once weekly to bi-weekly
-
Device: 0.5–1.0 mm rollers or pens
Minoxidil + microneedling = significantly better outcomes, even in the frontal zone. Just don’t overdo it—more pain ≠ more growth.
Platelet-Rich Plasma (PRP)
- Your blood, spun down and re-injected into the scalp
- Contains growth factors that stimulate dormant follicles
- Requires 3–6 sessions + maintenance every 4–6 months
- Evidence: RCTs confirm efficacy; results vary depending on protocol
Best for: Early-stage thinning or after surgical restoration to improve density at the edges.
Read More: How PRP therapy helps in hair growth?
Ketoconazole Shampoo
- Antifungal + anti-inflammatory
- May reduce scalp DHT activity
- Can be used 2–3 times/week alongside other treatments
- It’s like a scalp foundation—not a primary fix, but a helper
Tier 3: Procedural + Camouflage Options
Hairline Transplantation
- Follicular Unit Extraction (FUE) or Strip Method
- Ideal for stable AGA cases with good donor density
- Female design: rounded, lower, less aggressive temples
- Male design: conservative M-shape to future-proof against further loss
Pro tip: Overly aggressive hairlines often look great at 30… and bizarre at 45. Choose wisely.
Hairline Lowering Surgery
- Scalp advancement surgery
- Best for women with naturally high hairlines or forehead imbalance
- Not suitable for thinning or unstable scalp
Scalp Micropigmentation (SMP)
- Tattooing illusion of hair follicles
- Great for temple fill-ins, density illusion
- Zero regrowth—but significant aesthetic enhancement
Tier 4: Smart Camouflage
-
Keratin hair fibers: Temporary thickening effect; rain-resistant
-
Strategic parting: Move your part to camouflage thinner temples
-
Low-tension styles: Stop pulling your hairline into orbit. Give it a break.
-
LPT (Laser Phototherapy): Deserves its own section. (and that’s coming next.)
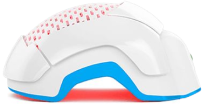
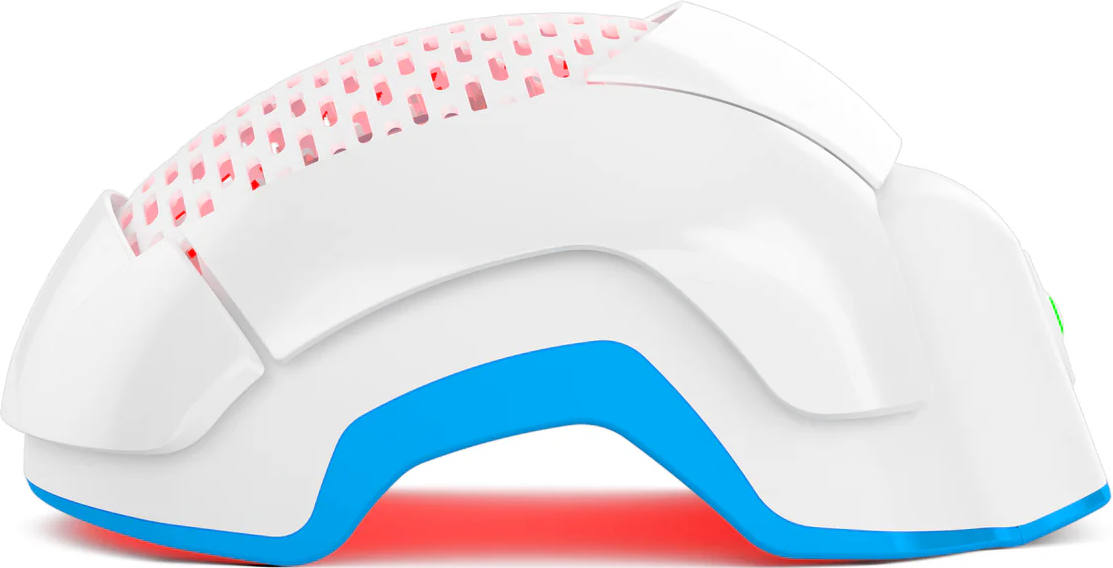
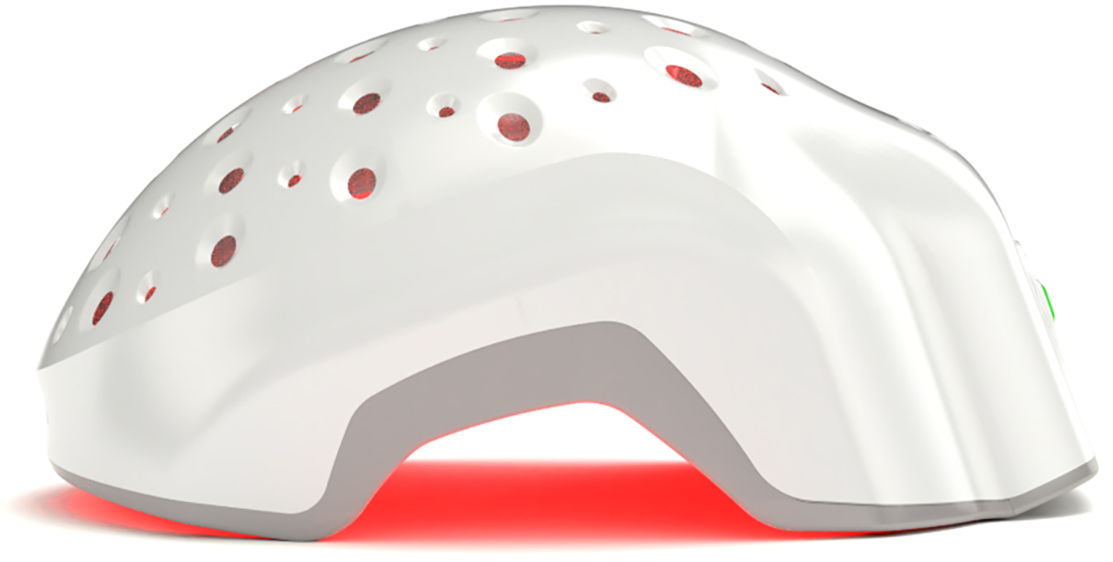
How Laser Phototherapy (LPT) Helps the Hairline
There’s a lot of chatter about red light, infrared, “LLLT” devices, laser combs, helmets, bands, caps, diodes, photons. People Google this stuff until their eyes cross.
But when it comes to non-invasive, evidence-backed treatments for frontal hairline stabilization, there’s one modality that deserves a very real spotlight:
Laser Phototherapy (LPT)
Yes. It works.
Yes. It’s FDA-cleared.
And yes—if you use the right device the right way—it can help your hairline too.
The Science
Laser Phototherapy works by delivering low-intensity, cool laser light directly to your scalp. While many devices use wavelengths around 650 nm, Theradome is engineered to use the clinically optimal 680 nm wavelength—shown to penetrate effectively into hair follicle tissue.
But wavelength alone isn’t enough. What makes Theradome different is the combination of:
- Maximum energy density: ensuring enough light actually reaches the follicles to trigger change.
- Laser coherence: unlike LEDs or diffuse light, coherent laser beams maintain their strength and precision, driving energy deeper.
-
IntelliDose™ technology: automatically calibrates each session so your scalp receives a precise, consistent “dose” of laser energy—never too little, never too much.
The result is reliable stimulation of follicle cells, increased ATP production, and improved blood flow—helping dormant hairs re-enter the growth phase while thickening existing strands.
The technical term is photobiomodulation.
What it means in human terms: the laser light energy gets absorbed by your scalp tissue. That stimulates mitochondrial activity (the little engines inside your cells), boosts ATP production, and increases blood flow to the follicle. Over time, this helps push resting (telogen) hairs back into active growth (anagen), while thickening the diameter of existing strands.
It’s like a growth nudge—but at the cellular level.
And unlike the surgical or hormonal options, this one’s completely drug-free, pain-free, and effortless.
Cold Lasers vs Scary Lasers
Let’s be honest—when people hear the word “laser,” they flinch.
Burns? Scars? Hollywood trauma?
Nope.
LPT uses Class 3R “cold” lasers, which deliver less than 5mW of optical power per diode. That’s about 20,000 times weaker than the light from a 100W bulb. These lasers don’t heat tissue. They don’t damage DNA. And they’ve been used safely in dermatology and physical therapy for over two decades.
To put it bluntly: if you’ve ever used a red laser pointer in a presentation, you’ve already been exposed to this class of laser.
Except LPT is tuned to help hair—not to chase your cat around the living room.
So… Does LPT Work on the Hairline?
Yes—especially if you start early.
Most of the strongest data on LPT historically focused on crown and vertex regions. That’s because they’re easier to photograph, count, and standardize in trials. But more recent studies, including sham-controlled RCTs, show that LPT can increase terminal hair density across the entire scalp, including frontal and temporal zones.
Consistency is key. As with all therapies, the hairline takes time to respond. Expect:
- 3–4 months: reduced shedding
- 4–6 months: signs of new vellus growth
- 6–12 months: improved density, coverage, and texture
And if you're pairing LPT with something like minoxidil or microneedling? Even better.
When to Seek Help from a Hair Specialist
You’ve done the photos. You’ve stared in the mirror. You’ve even tried the “maybe it’s just the lighting” excuse.
So—when do you cross the line from casual monitoring to professional intervention?
Here’s a short list of signs it’s time to see a trichologist or dermatologist:
- The recession is rapid, not slow and steady.
- You’re noticing itching, burning, or visible redness around the hairline.
- You’re losing eyebrows or experiencing hair loss in other body areas.
- Your frontal edge is no longer showing baby hairs—but instead looks shiny or barren.
- You’ve tried over-the-counter solutions for more than 6 months… with no meaningful shift.
And the earlier you act, the more options are on the table.
Especially with conditions like FFA or scarring alopecias, where the window for intervention can close permanently if you wait too long.
What to Expect at the Appointment
- Scalp exam (under normal light + trichoscope)
- Medical history (including family patterns, hormonal shifts, recent stress)
- Photos for baseline comparison
- Possibly a scalp biopsy if scarring is suspected
What to bring:
- Timeline of symptoms
- Products you're using
- Old photos (if available)
- Patience… and curiosity
You don’t need to walk in with a diagnosis. That’s their job. Yours is to notice the shift and show up early enough for real solutions to still work.
Conclusion
Here’s the thing nobody says out loud:
Your hairline isn’t your worth.
Yes, it frames your face. Yes, it can shift how you feel when you see yourself. But whether it’s rounded, V-shaped, subtly thinning, or bouncing back with a vengeance—it doesn’t change the core of who you are.
Still, that doesn’t mean you have to just “accept” change if it’s bothering you. Science exists for a reason. We have tools (powerful, proven, precise ones) that can slow, stabilize, or even rebuild what’s been lost.
You just need to catch the signals early.
To trust evidence over influencers.
To remember that new baby hairs count, too.
So here’s your action plan:
- Step 1: Assess with clarity.
- Step 2: Choose smart, safe interventions.
- Step 3: Stick with them long enough to matter.
And if all else fails? Adjust the lighting, part your hair the other way, take a breath… and come back to the science.
Because your hairline doesn’t need to be perfect.
It just needs to be understood.